Labor and Delivery
Overview
What is labor and delivery?
The process that leads to childbirth is called labor and delivery. There are three stages of labor. In the first stage, uterine contractions help thin and open the cervix. The second stage is the actual birth. The third stage is delivery of the placenta.
How can you manage pain?
Your pain relief choices for childbirth may include medical and nonmedical treatments. Medical choices can include I.V. medicines or epidural pain relief. Massage and focused breathing are some of the nonmedical options. Sometimes both kinds of pain relief are used. Knowing your options can help you prepare for childbirth.
How can you prepare for labor and delivery?
You can get ready for labor and delivery by taking a childbirth education class and writing a birth plan. A childbirth class can help reduce your stress both before and during labor and delivery. A birth plan tells others what your wishes are for your labor and delivery.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Planning for Birth
Two good ways to prepare yourself for labor and delivery are by taking a childbirth education class and writing a birth plan.
- Childbirth education class.
-
A childbirth education class can reduce your stress both before and during labor and delivery. That's because the class can prepare you to deal with what might happen.
A good time to start the class is in your sixth or seventh month of pregnancy. If your partner or a friend is going to be your labor coach, they can come too.
- Birth plan.
-
A birth plan is a document that states your wishes for labor and delivery. It includes who and where you'd like to deliver your baby and what kinds of pain relief you'd like to try. You can give copies of your plan to your doctor or midwife, your support person, and the hospital or birthing center.
Writing a birth plan
A birth plan lets you write down your vision of an ideal birth and share it with your support person, the hospital or birth center, and your doctor or midwife.
Your birth may not go as planned. But the process of making a plan can be a great way to get everyone on the same page about what you think you'd prefer.
Here are some ideas for making a birth plan.
- Choose where you want to have your baby.
It could be a hospital, a birthing center, or your home. The setting may depend on your level of risk for problems during delivery, and if you're working with a doctor or midwife.
- List the comfort measures you want to try.
Think breathing techniques, laboring in water, or trying different positions.
- Include the medical treatments you prefer to have.
Think about pain medicine you'd want, even if you don't think you'll need it. And think about your options if you end up needing a C-section.
- Say how you want your baby to be cared for after delivery.
- You might want your baby to stay in the room with you rather than in the nursery.
- You might want to delay some tests so you can hold your baby and start breastfeeding right away.
- List who you want to be there with you.
Maybe you want family and friends in the room, or maybe you only want the baby's other parent or a support person like a doula.
As you think about your plan, give yourself permission to be flexible. It's hard to know what will happen. The most important thing is to make sure you and your baby are healthy and safe.
Learn more
Signs of Labor
Late in your pregnancy, your doctor or midwife will tell you what to do when you think you are in labor. At first, your contractions may not be regular and may happen only now and then.
You may have signs that early labor is not far off.
- The baby may settle into your pelvis. Although this is called dropping, or lightening, you may not feel it.
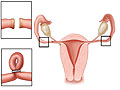
- Your cervix may begin to thin and open (cervical effacement and dilation). Your doctor may check for this during your prenatal exams.
- Braxton Hicks contractions may become painful, more frequent, and stronger. You may also feel cramping in the groin or rectum or an ongoing ache low in your back.
- Your amniotic sac may break (rupture of the membranes). In most cases, rupture of the membranes occurs after labor has already started. In some people, this happens before labor starts. Call your doctor or midwife immediately or go to the hospital if your membranes have ruptured.
When you're in labor, the contractions get longer, stronger, and closer together. You will feel them even when you change positions and walk or move around. After a while, it will become hard for you to talk during a contraction. You may have to stop to focus on your breathing.
When to call a doctor
Call 911 anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have a seizure.
- You have severe vaginal bleeding.
- You have severe pain in your belly or pelvis that doesn't get better between contractions.
- You have had fluid gushing or leaking from your vagina and you know or think the umbilical cord is bulging into your vagina. If this happens, immediately get down on your knees so your rear end (buttocks) is higher than your head. This will decrease the pressure on the cord until help arrives.
Call your doctor now or seek immediate medical care if:
- You have new or worse signs of preeclampsia, such as:
- Sudden swelling of your face, hands, or feet.
- New vision problems (such as dimness, blurring, or seeing spots).
- A severe headache.
- You have any vaginal bleeding.
- You have belly pain or cramping.
- You have a fever.
- You have had regular contractions (with or without pain) for an hour. This means that you have 8 or more within 1 hour or 4 or more in 20 minutes after you change your position and drink fluids.
- You have a sudden release of fluid from your vagina.
- You have low back pain or pelvic pressure that does not go away.
- You notice that your baby has stopped moving or is moving much less than normal.
Watch closely for changes in your health, and be sure to contact your doctor if you have any problems.
Learn more
Watch
Managing Pain
You have many choices to relieve pain during childbirth. These include medical and nonmedical options. You may use more than one of these choices.
Nonmedical
Nonmedical options may help reduce pain and help you feel a sense of control during labor. These techniques include:
- Support. Having a support person with you through childbirth may help you manage your pain better. This person could be your partner, a loved one, or a friend. Or you may use an experienced birth assistant, like a doula, whose only job is to give you constant support.
- Distraction. During early labor, you can walk, play cards, watch TV, take a shower, or listen to music to help take your mind off your contractions.
- Massage. Massage of the shoulders and lower back during contractions may help ease your pain.
- Changing positions during labor. Walking, kneeling, or sitting on a big rubber ball (birth ball) are good options. The position that feels best may change as you move through labor.
- Focused breathing techniques. Breathing in a rhythm can distract you from pain and relax your muscles and your mind. Childbirth education classes can teach you different methods of focused breathing.
- Imagery. This involves using your imagination to decrease your pain. For instance, you could imagine your contractions as waves rolling over you. Picture a peaceful place, such as a beach or a mountain stream, to help you relax between contractions.
- Laboring in water. Some hospitals and birthing centers offer tubs or whirlpools for labor. Soaking in warm water may help ease the stress of labor.
Other techniques that don't use medicine to control pain include hypnosis and acupuncture.
Medical
Your options for pain relief with medicine may include:
- I.V. medicines. Examples include fentanyl and hydroxyzine. These medicines are used to help reduce anxiety and partially relieve pain. But they aren't usually used when you are close to delivery, because they can affect a newborn's breathing.
- Spinal and epidural pain relief. This is a shot (spinal) or an ongoing supply (epidural) of pain medicine near the spinal cord. It partially or fully numbs the belly and lower body.
- Pudendal block. This is a shot of pain medicine to numb the vagina and perineum. It can help relieve pain from the second (pushing) stage of labor. It works quickly and usually doesn't affect the baby.
- Nitrous oxide. You can give yourself nitrous oxide through a mouthpiece or mask when you need pain relief during labor. You can decide when to use it.
Learn more
Watch
Types of Delivery
Vaginal birth
Vaginal birth means delivering a baby through the birth canal (vagina). During labor, the uterus tightens (contracts) regularly to thin and open the cervix and to push the baby out through the birth canal. It can take many hours or sometimes days for the cervix to open all the way so you can begin pushing. Most babies are born by vaginal delivery.
Cesarean section
Cesarean section (C-section) is the delivery of a baby through a cut (incision) in your belly and uterus. In most cases, you can be awake during the birth and be with your newborn soon afterward. It can take 4 to 6 weeks to recover completely from the surgery.
A C-section may be planned or unplanned. In most cases, doctors do cesarean sections because of problems that arise during labor.
Vaginal birth after cesarean
Vaginal birth after cesarean (VBAC) means delivering a baby through the birth canal after having had a C-section for a previous birth. In the past, if you had one baby by C-section, you had to have your next babies by C-section. But now you may be able to try for a vaginal birth. It depends on the reason for the first C-section and the type of incision that was made.
Learn more
Watch
Stages of Labor
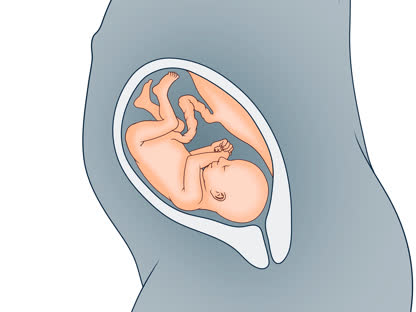
There are three stages of labor that can occur over many hours or even a few days. The first stage is labor. During the second stage, you deliver the baby. The final stage is delivering the placenta.
First stage of labor
The first stage of labor is divided into three phases: early labor, active labor, and transition.
Early labor
Early labor is often the longest part of the birthing process, sometimes lasting 2 to 3 days. Contractions:
- Are mild to moderate (you can talk while they are happening) and last about 30 to 45 seconds.
- May be irregular (5 to 20 minutes apart) and may even stop for a while.
- Open (dilate) the cervix to about 4 cm (1.6 in.) to 6 cm (2.4 in.). Those who are delivering for the first time can have many hours of early labor without the cervix dilating.
It's common for those in early labor to go to the hospital and be sent home until they are in active labor or until their "water" (amniotic sac) breaks.
Active labor
Active labor starts when the cervix is about 5 cm (2 in.) to 6 cm (2.4 in.) dilated. This stage is complete when the cervix is fully effaced and dilated and the baby is ready to be pushed out.
During this phase, contractions get stronger, are more frequent (every 2 to 3 minutes), and last longer (50 to 70 seconds). Now is the time to be at or go to the hospital or birthing center. If your amniotic sac hasn't broken before this, it may now.
You may be restless and excited, and you may feel the need to shift positions often. This is good because it improves your circulation.
As your contractions get stronger:
- You may want to use comfort measures, such as breathing techniques or massage, to control pain and anxiety. Or you may want medicine for pain, such as epidural anesthesia.
- You may be given intravenous (I.V.) fluids.
Transition
Transition is the end of active labor. As the baby moves down, contractions become more intense and longer and come even closer together. Delivery isn't far off.
During transition, you may be self-absorbed, focused on what your body is doing. You may want others nearby for support but be annoyed or distracted by their attempts to help. You may feel more and more anxious, nauseated, exhausted, or fearful.
If you're delivering for the first time, transition may take up to 3 hours. If you've had a vaginal birth before, it will usually take no more than an hour. Some people have a very short and intense transition.
Second stage of labor
The second stage is the actual birth, when the baby is pushed out by the contractions. This pushing stage can be as short as a few minutes or as long as several hours. You are more likely to have a fast labor if you have given birth before.
In the second stage:
- Your contractions may feel different. They are usually regular, but they may slow down to every 2 to 5 minutes and last 60 to 90 seconds.
- You may have a strong urge to push or bear down with each contraction.
- You may need to change position several times to find the right birthing position for you.
You may feel a burning pain when your baby's head comes through the vagina (crowns). You can have a mirror positioned so you can watch your baby's head crown.
If the baby is coming quickly, your doctor or midwife may ask you not to push with every contraction. This may give the perineum a chance to stretch without tearing.
Then after a final push, your baby is born, and you get to hold and look at this new person for the first time. But your body still has some work to do: stage three, delivery of the placenta.
Third stage of labor
The third stage of labor is when the placenta is delivered. You will still have contractions. They make the placenta separate from the inside of the uterus, and they push the placenta out.
The third stage can be as quick as 5 minutes. But in most cases, the placenta is delivered within 30 minutes. Your contractions will continue until after the placenta is delivered, so you may have to focus and breathe until this uncomfortable process is complete.
Your care provider will help you during this time. If the placenta doesn't fully detach, your doctor or midwife may remove by hand what's left inside. You'll also be watched for any problems, such as heavy bleeding, especially if you have had it before.
You may be given medicine after the placenta is delivered. Oxytocin (such as Pitocin) is used to make the uterus shrink and bleed less. (This is the same medicine that is sometimes used to make contractions more regular and frequent during labor.) Breastfeeding right away can also help the uterus shrink and bleed less.
Labor Positions
In most cases, you don't have to lie in bed while you're in labor. Your nurse or doctor may have you stay in bed or in a certain position if there are problems with your baby or your health. Or you may need to be in bed if you have an epidural.
If you don't need to be in bed, you can choose whichever position feels most comfortable. You may want to walk, sit on a big rubber ball, or kneel. The position that feels best for you may change as you move through labor.
Moving around and changing positions during labor may help you feel more comfortable.
Walking

During early labor, walking can help ease discomfort or pain. Some people walk during much of their labor.
Leaning

Leaning forward during each contraction can help ease discomfort or pain.
Sitting

Sitting backward in a chair and leaning over the back of a chair is a comfortable position that lets you rest while staying upright. You can place a pillow between your belly and the chair back. Leaning over the back of a chair is also a good position for receiving a back rub.
Squatting

Squatting opens the pelvis, especially when you hold onto something stable and stretch away from it. This position can be used for pushing during contractions and for delivering the baby.
Kneeling

Kneeling over a chair, ball, or cushions is good for active labor and for when you need to rest. This position is easy to move into and out of when you feel the need to change position. You may find it eases back labor.
Kneeling on hands and knees

Kneeling on your hands and knees can be used to reduce the intensity of contractions and to try to turn a posterior-facing baby. You may find that kneeling eases back labor.
Downward from knees

Lowering yourself from hands-and-knees can help ease the physical and emotional intensity of labor. It is also used to take pressure off of the back and may help shift a baby to a more favorable position. You may find that it eases back labor.
Side-lying

Lying on your side can give you needed rest during a long labor. Take care to prop up your upper leg and head.
Birthing positions during the pushing stage
Birthing positions for pushing include squatting, reclining, and using a birthing chair, stool, or bed. You may find that certain positions are more comfortable than others during the pushing stage. Speak to your doctor or midwife about different birthing positions before your labor begins.
- Kneeling, getting down on your hands and knees, or leaning onto a birthing ball may help to take pressure off your back.
- Squatting feels comfortable for some people.
- Lying on your back in a semi-reclining position with your legs supported by stirrups is a common birthing position used in the United States. While pushing, your doctor or midwife may have you grab behind your knees and pull up.
- Lying on your side is another option.
- Some birthing centers use a birthing stool or chair during the pushing stage. A birthing chair may help you feel more comfortable.
Medical Procedures
Some exams and procedures are normally done during labor. Others are used as needed.
- Sterile vaginal exams.
-
These are done to check how much your cervix has thinned and opened.
- Fetal heart monitoring.
-
Your baby's heart rate will be checked during labor. The heart rate is a good sign of how your baby is doing. Fetal heart monitoring may be done at set times (intermittent) or all the time (continuous).
- Labor induction.
-
Measures may be taken to start (induce) labor. This may be done by breaking (rupturing) the amniotic sac. Or medicine may be used to soften the cervix or cause contractions. These measures may be needed if labor doesn't start on its own and the baby needs to be delivered soon. They may also be used if active labor starts on its own but contractions slow or stop.
- Antibiotics.
-
You will be given antibiotics if you tested positive for group B strep during your pregnancy.
In some cases, a woman may need medical help to give birth.
- Delivery assistance.
-
Forceps delivery or vacuum extraction can be used to assist a vaginal delivery. This may be needed at the pushing stage if labor is stalled. It may also be done if the baby shows signs of distress and needs to be delivered quickly.
- Episiotomy.
-
An episiotomy is a cut (incision) to widen the perineum. This is sometimes done to deliver the baby's head more quickly, when there are signs of distress.
Sometimes what starts as a routine vaginal birth may end in a cesarean delivery (C-section). This may be done to make sure the mom and baby are safe.
Learn more
Right After the Birth
The first hours after childbirth
You may have shaking chills right after delivery. This is a common reaction in the hours after delivery. A warm blanket may help you feel more comfortable.
During the first hours after the birth, your health professional or a nurse will:
- Massage your uterus by rubbing your lower belly about every 15 minutes. Later, you will be taught to massage your own uterus. This helps it tighten (contract) and stop bleeding.
- Check your bladder to make sure it isn't full. A full bladder puts pressure on your uterus, which interferes with contractions. You will be asked to try to urinate. This may be hard because of pain and swelling. If you can't urinate, a tube (catheter) can be used to empty your bladder.
- Check your blood pressure often.
- Repair the area between your vagina and anus (perineum) if it tore or if you had an incision (episiotomy).
- Remove the small tube in your back if you had epidural anesthesia. If you plan to have a tubal ligation surgery to prevent future pregnancy, the tube may be left in.
Bonding with your newborn
Close physical contact helps you bond with your baby and helps your newborn feel secure. One special way to bond with your newborn is "kangaroo care." This simply means holding your baby to your chest, skin to skin. Talking to, reading to, and caring for your baby also help to form a bond.
If you plan to breastfeed
It's best to start breastfeeding within 1 hour of birth. For each feeding:
- Get ready. Try to relax. Have some water or juice and support pillows ready.
- Find a position that's comfortable for you and your baby. Make sure the baby's head and chest are lined up straight and facing your breast. It's best to switch which breast you start with each time.
- Get the baby latched on well. Your baby's mouth should be wide open, so you may need to gently touch the middle of your baby's lower lip. When your baby's mouth is open wide, quickly bring the baby onto your nipple and areola.
- Let your baby decide how long to nurse. Burp your baby after each breast.
Breastfeeding doesn't always come easily at first. But it gets better with practice. Be patient. Talk to your doctor, midwife, or lactation specialist if you have problems.
Learn more
Watch
Related Information
Credits
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.