Adult Primary Liver Cancer Treatment: Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
What Is Liver Cancer?
Primary liver cancer is a disease in which malignant (cancer) cells form in the tissues of the liver. Cancer that forms in other parts of the body and spreads to the liver is not primary liver cancer. The liver is one of the largest organs in the body. It has two lobes and fills the upper right side of the abdomen inside the rib cage. The main functions of the liver include the following:
- to make bile to help digest fat that comes from food
- to store glycogen (sugar), which the body uses for energy
- to filter harmful substances from the blood so they can be passed from the body in stools and urine
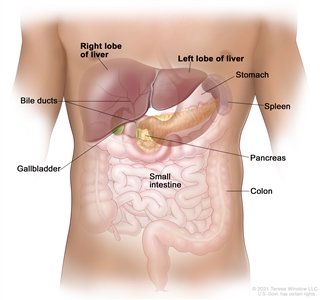
Anatomy of the liver. The liver is in the upper abdomen near the stomach, intestines, gallbladder, and pancreas. The liver has a right lobe and a left lobe. Each lobe is divided into two sections (not shown).
Types of liver cancer
Hepatocellular carcinoma and bile duct cancer (cholangiocarcinoma) are the main types of adult primary liver cancer.
Most adult primary liver cancers are hepatocellular carcinomas. This type of liver cancer is the third leading cause of cancer-related deaths worldwide.
Primary liver cancer can occur in both adults and children. However, treatment for children is different than treatment for adults. For more information, see Childhood Liver Cancer.
Signs and symptoms of liver cancer
These and other signs and symptoms may be caused by adult primary liver cancer or by other conditions. Check with your doctor if you have any of the following:
- a hard lump on the right side just below the rib cage
- discomfort in the upper abdomen on the right side
- a swollen abdomen
- pain near the right shoulder blade or in the back
- jaundice (yellowing of the skin and whites of the eyes)
- easy bruising or bleeding
- unusual tiredness or weakness
- nausea and vomiting
- loss of appetite or feelings of fullness after eating a small meal
- weight loss for no known reason
- pale, chalky bowel movements and dark urine
- fever
How is liver cancer diagnosed?
Tests that examine the liver and the blood are used to detect and diagnose liver cancer. Every person will not receive all the tests described below.
The following tests and procedures may be used:
- Physical exam and health history: A physical exam of the body will be done to check a person's health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
- Alpha-fetoprotein (AFP) tumor marker test: Tumor markers are released into the blood by organs, tissues, or tumor cells in the body. An increased level of AFP in the blood may be a sign of liver cancer. Other cancers and certain noncancerous conditions, including cirrhosis and hepatitis, may also increase AFP levels. Sometimes the AFP level is normal even when there is liver cancer.
- Liver function tests: These blood tests measure the amounts of certain substances released into the blood by the liver. A higher-than-normal amount of a substance can be a sign of liver cancer.
- CT scan (CAT scan): This procedure uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, such as the abdomen, taken from different angles. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Images may be taken at three different times after the dye is injected, to get the best picture of abnormal areas in the liver. This is called triple-phase CT. A spiral or helical CT scan makes a series of very detailed pictures of areas inside the body using an x-ray machine that scans the body in a spiral path.
- Magnetic resonance imaging (MRI): This procedure uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body, such as the liver. To create detailed pictures of blood vessels in and near the liver, dye is injected into a vein. This procedure is called magnetic resonance angiography. Images may be taken at three different times after the dye is injected, to get the best picture of abnormal areas in the liver. This is called triple-phase MRI.
- Ultrasound exam: This procedure uses high-energy sound waves (ultrasound) that are bounced off the liver and make echoes. The echoes form a picture of the liver called a sonogram.
-
Biopsy: During a biopsy, cells or tissues are removed so they can be viewed under a microscope by a pathologist to check for signs of cancer. Procedures used to collect the sample of cells or tissues include the following:
- Fine-needle aspiration biopsy: A sample of fluid, tissue, or cells is removed using a thin needle.
- Core needle biopsy: A sample of cells or tissue is removed using a slightly wider needle.
- Laparoscopy: This surgical procedure is done to look at the organs inside the abdomen to check for signs of disease. Small incisions (cuts) are made in the wall of the abdomen and a laparoscope (a thin, lighted tube) is inserted into one of the incisions. Another instrument is inserted through the same or another incision to remove the tissue samples.
A biopsy is not always needed to diagnose liver cancer. Sometimes the doctors can diagnose liver cancer based on the results of imaging tests such as CT scans and MRI.
After primary liver cancer has been diagnosed, tests are done to find out if cancer cells have spread within the liver or to other parts of the body. The process of determining the size and location of the cancer and whether it has spread is called staging.
Some of the tests and procedures used to diagnose liver cancer, such as CT scan and MRI, may be used in the staging process. A positron emission tomography (PET) scan may also be used:
- PET scan: This procedure is used to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do.
What affects liver cancer prognosis?
Once liver cancer has been diagnosed, the prognosis (chance of recovery) and treatment options depend on the following:
- the stage of the cancer (the size of the tumor, whether it affects part or all of the liver, or has spread to other places in the body)
- how well the liver is working
- the patient's general health, including whether there is cirrhosis of the liver
Finding and treating liver cancer early may prevent death from liver cancer.
Liver Cancer Stages
This page describes the stages of liver cancer for adults. The stage describes the extent of cancer in the body. Knowing the stage of liver cancer helps the doctor plan the best treatment.
To learn about liver cancer stages for children, see Stages of hepatoblastoma.
To learn about the tests and procedures used to diagnose and stage primary liver cancer, see Liver Cancer Diagnosis.
There are several staging systems for liver cancer. The Barcelona Clinic Liver Cancer (BCLC) Staging System is widely used to stage primary liver cancer. The system is used to predict the patient's chance of recovery and to plan treatment, based on the following:
- whether the cancer has spread within the liver or to other parts of the body
- how well the liver is working
- the general health and wellness of the patient
- the symptoms caused by the cancer
The BCLC staging system has five stages:
- stage 0: very early
- stage A: early
- stage B: intermediate
- stage C: advanced
- stage D: end-stage
For liver cancer in adults, stages are also grouped according to how the cancer may be treated:
- Localized liver cancer has not spread outside the liver and can be removed by surgery. This includes BCLC stages 0, A, and B.
- Locally advanced liver cancer has not spread from the liver to distant parts of the body but cannot be safely removed by surgery. This includes BCLC stage C.
- Metastatic liver cancer is cancer that has spread from the liver to distant parts of the body. Metastatic liver cancer cannot be completely removed by surgery. This includes BCLC stage D. To learn more about metastatic cancer, see Metastatic Cancer: When Cancer Spreads.
- Recurrent liver cancer is cancer that came back after treatment. The cancer may come back in the liver or in other parts of the body. To learn more about recurrent cancer, see Recurrent Cancer: When Cancer Comes Back.
To learn about other ways cancer stages can be described, see Cancer Staging.
To learn about treatment options, see Liver Cancer Treatment.
Liver Cancer Treatment
There are different types of treatment for people with liver cancer. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials.
Types of treatment
Surveillance
Surveillance is used for lesions smaller than 1 centimeter found during screening. Follow-up every 3 months is common. Surveillance is closely watching a person's condition but not giving any treatment unless there are changes in test results that show the condition is getting worse. During active surveillance, certain exams and tests are done on a regular schedule.
Surgery
A partial hepatectomy (surgery to remove the part of the liver where cancer is found) may be done. A wedge of tissue, an entire lobe, or a larger part of the liver, along with some of the healthy tissue around it is removed. The remaining liver tissue takes over the functions of the liver and may regrow.
Liver transplant
In a liver transplant, the entire liver is removed and replaced with a healthy donated liver. A liver transplant may be done when the disease is in the liver only and a donated liver can be found. If the person has to wait for a donated liver, other treatment is given as needed.
Ablation therapy
Ablation therapy removes or destroys tissue. Different types of ablation therapy are used for liver cancer:
- Radiofrequency ablation: Special needles are inserted directly through the skin or through an incision in the abdomen to reach the tumor. High-energy radio waves heat the needles and tumor which kills cancer cells.
- Microwave therapy: The tumor is exposed to high temperatures created by microwaves. This can damage and kill cancer cells or make them more sensitive to the effects of radiation and certain anticancer drugs.
- Percutaneous ethanol injection: A small needle is used to inject ethanol (pure alcohol) directly into a tumor to kill cancer cells. Several treatments may be needed. Usually local anesthesia is used, but if the person has many tumors in the liver, general anesthesia may be used.
- Cryoablation: An instrument is used to freeze and destroy cancer cells. This type of treatment is also called cryotherapy and cryosurgery. The doctor may use ultrasound to guide the instrument. Learn more at Cryosurgery to Treat Cancer.
- Electroporation therapy: Electrical pulses are sent through an electrode placed in a tumor to kill cancer cells. Electroporation therapy is being studied in clinical trials.
Embolization therapy
Embolization therapy is used for people who cannot have surgery to remove the tumor or ablation therapy and whose tumor has not spread outside the liver. Embolization therapy is the use of substances to block or decrease the flow of blood through the hepatic artery to the tumor. When the tumor does not get the oxygen and nutrients it needs, it will not continue to grow.
The liver receives blood from the hepatic portal vein and the hepatic artery. Blood that comes into the liver from the hepatic portal vein usually goes to the healthy liver tissue. Blood that comes from the hepatic artery usually goes to the tumor. When the hepatic artery is blocked during embolization therapy, the healthy liver tissue continues to receive blood from the hepatic portal vein.
There are two main types of embolization therapy:
- Transarterial embolization (TAE): A small incision (cut) is made in the inner thigh and a catheter (thin, flexible tube) is inserted and threaded up into the hepatic artery. Once the catheter is in place, a substance that blocks the hepatic artery and stops blood flow to the tumor is injected.
- Transarterial chemoembolization (TACE): This procedure is like TAE except an anticancer drug is also given. The procedure can be done by attaching the anticancer drug to small beads that are injected into the hepatic artery or by injecting the anticancer drug through the catheter into the hepatic artery and then injecting the substance to block the hepatic artery. Most of the anticancer drug is trapped near the tumor and only a small amount of the drug reaches other parts of the body. This type of treatment is also called chemoembolization.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies used to treat advanced liver cancer include:
- bevacizumab
- cabozantinib
- lenvatinib
- ramucirumab
- regorafenib
- sorafenib
Learn more about targeted therapy and its side effects at Targeted Therapy to Treat Cancer.
Immunotherapy
Immunotherapy is a treatment that uses the person's immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body's natural defenses against cancer.
Immune checkpoint inhibitors are a type of immunotherapy. Immune checkpoint inhibitors that may be used to treat liver cancer include:
- atezolizumab with the targeted therapy drug bevacizumab or cabozantinib
- durvalumab with tremelimumab
- nivolumab with ipilimumab
- pembrolizumab
Learn more about immunotherapy and its side effects at Immunotherapy to Treat Cancer and Immunotherapy Side Effects.
Radiation therapy
External radiation therapy uses a machine outside the body to send high-energy x-rays or other types of radiation toward the area of the body with cancer. Radiation is given in a series of treatments to allow healthy cells to recover and to make radiation more effective. The number of treatments is based on details about the cancer, such as the size and location of the tumor. Certain ways of giving external radiation therapy can help keep radiation from damaging nearby healthy tissue:
- Conformal radiation therapy: Conformal radiation therapy uses a computer to make a 3-dimensional, or 3-D, picture of the tumor and shapes the radiation beams to fit the tumor. This allows a high dose of radiation to reach the tumor and causes less damage to nearby healthy tissue.
- Stereotactic body radiation therapy: Stereotactic body radiation therapy uses special equipment to place the person in the same position for each radiation treatment. Once a day for several days, a radiation machine aims a larger than usual dose of radiation directly at the tumor. By having the person in the same position for each treatment, there is less damage to nearby healthy tissue. This procedure is also called stereotactic external-beam radiation therapy and stereotaxic radiation therapy.
- Proton beam radiation therapy: Proton beam radiation therapy is a type of high-energy, external radiation therapy that uses streams of protons (tiny particles with a positive charge) to kill tumor cells. This type of treatment can lower the amount of radiation damage to healthy tissue near a tumor.
Learn more about radiation therapy and its side effects at Radiation Therapy to Treat Cancer and Radiation Therapy Side Effects.
Clinical trials
For some people, joining a clinical trial may be an option. There are different types of clinical trials for people with cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Clinical Trials Information for Patients and Caregivers.
Treatment of localized liver cancer
Treatment of localized liver cancer may include:
- surveillance for lesions smaller than 1 centimeter
- partial hepatectomy (surgery to remove the part of the liver where cancer is found)
- liver transplant
- ablation of the tumor using:
- radiofrequency ablation
- microwave therapy
- percutaneous ethanol injection
- cryoablation
- radiation therapy
Treatment of locally advanced or metastatic liver cancer
Treatment of locally advanced or metastatic liver cancer may include:
- transarterial embolization (TAE) or transarterial chemoembolization (TACE) in people with locally advanced liver cancer
- bevacizumab, cabozantinib, lenvatinib, ramucirumab, regorafenib, or sorafenib
- atezolizumab with bevacizumab or cabozantinib, durvalumab with tremelimumab, nivolumab with ipilimumab, or pembrolizumab
- radiation therapy
Treatment of recurrent liver cancer
Treatment options for recurrent primary liver cancer may include:
- total hepatectomy (surgery to remove all of the liver) and liver transplant
- partial hepatectomy (surgery to remove the part of the liver where cancer is found)
- ablation therapy
- transarterial chemoembolization (TACE) and sorafenib as palliative therapy to relieve symptoms and improve quality of life
Last Revised: 2024-05-15
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.


