Acute Myeloid Leukemia Treatment (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Acute Myeloid Leukemia
Adult acute myeloid leukemia (AML) is a type of cancer in which the bone marrow makes a large number of abnormal blood cells.
AML is a cancer of the blood and bone marrow. It is the most common type of acute leukemia in adults. This type of cancer usually gets worse quickly if it is not treated. AML is also called acute myelogenous leukemia and acute nonlymphocytic leukemia.
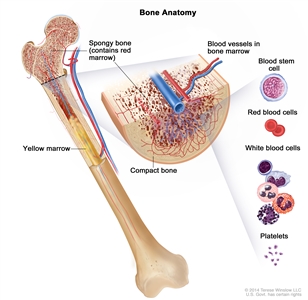
Anatomy of the bone. The bone is made up of compact bone, spongy bone, and bone marrow. Compact bone makes up the outer layer of the bone. Spongy bone is found mostly at the ends of bones and contains red marrow. Bone marrow is found in the center of most bones and has many blood vessels. There are two types of bone marrow: red and yellow. Red marrow contains blood stem cells that can become red blood cells, white blood cells, or platelets. Yellow marrow is made mostly of fat.
Leukemia may affect red blood cells, white blood cells, and platelets.
The bone marrow makes blood stem cells (immature cells) that become mature blood cells over time. A blood stem cell may become a myeloid stem cell or a lymphoid stem cell.
Myeloid stem cells go through several stages of development in the bone marrow before fully maturing into:
- red blood cells that carry oxygen and other substances to all tissues of the body
- granulocytes and other types of white blood cells that help the body's immune system respond to infection, allergens, and inflammation
- platelets that help stop bleeding by forming clots
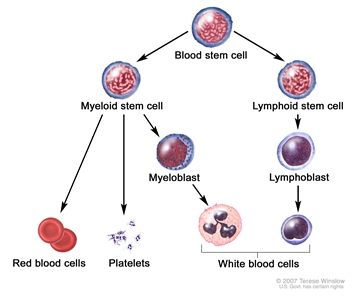
Blood cell development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell.
In AML, there is an increase in the number of immature white blood cells called myeloblasts (or myeloid blasts). The myeloblasts in AML are abnormal and do not become healthy white blood cells. As the number of these cells, also called leukemia cells, increases in the blood and bone marrow, there is less room for healthy platelets, red blood cells, and other white blood cells. This may lead to easy bleeding, anemia, and infection.
The leukemia cells can spread outside the blood to other parts of the body, including the central nervous system (CNS; brain and spinal cord), skin, and gums. Sometimes leukemia cells form a solid tumor called a myeloid sarcoma. Myeloid sarcoma is also called extramedullary myeloid tumor, granulocytic sarcoma, or chloroma.
There are different subtypes of AML.
Most AML subtypes are based on how mature (developed) the cancer cells are at the time of diagnosis, and how different they are from normal cells.
Acute promyelocytic leukemia (APL) is a subtype of AML. This leukemia occurs when genes on chromosome 15 switch places with some genes on chromosome 17, and an abnormal gene called PML::RARA is made. The PML::RARA gene sends a message that stops promyelocytes (a type of white blood cell) from maturing. Problems with severe bleeding and blood clots may occur. This is a serious health problem that needs treatment as soon as possible. APL usually occurs in middle-aged adults.
Smoking, previous chemotherapy treatment, and exposure to radiation may increase the risk of AML.
AML is caused by certain changes to the way blood stem cells function, especially how they grow and divide into new cells. A risk factor is anything that increases the chance of getting a disease. Some risk factors for AML, like smoking, can be changed. However, risk factors also include things people cannot change, like their genetics, getting older, and their health history.
There are many risk factors for AML, but many do not directly cause cancer. Instead, they increase the chance of DNA damage in cells that may lead to AML. Learn more about how cancer develops at What Is Cancer?
Having one or more of these risk factors does not mean that you will get AML. Many people with risk factors never develop AML, while others with no known risk factors do.
Possible risk factors for AML include:
- being male
- older age
- smoking
- having had treatment with chemotherapy or radiation therapy in the past
- being exposed to radiation in the environment (such as nuclear radiation) or to the chemical benzene
- having a personal history of a blood disorder such as myelodysplastic syndrome
- having certain syndromes or inherited disorders
Talk with your doctor if you think you may be at risk.
Signs and symptoms of AML include fever, feeling tired, and easy bruising or bleeding.
The early signs and symptoms of AML may be like those caused by the flu or other common diseases. Check with your doctor if you have:
- weakness or feeling tired
- fever
- infection
- paleness or loss of normal skin color
- bleeding
Less common signs or symptoms may be caused by clusters of leukemia cells in the CNS or testicles, or a tumor of myeloid cells called a chloroma.
Symptoms of acute leukemia often develop between 4 and 6 weeks before diagnosis.
Tests that examine the blood and bone marrow are used to diagnose AML.
In addition to asking about your personal and family health history and doing a physical exam, your doctor may perform the following tests and procedures:
-
Complete blood count (CBC) checks a sample of blood for:
- the number of red blood cells and platelets
- the number and type of white blood cells
- the amount of hemoglobin (the protein that carries oxygen) in the red blood cells
- the amount of hematocrit (whole blood that is made up of red blood cells)
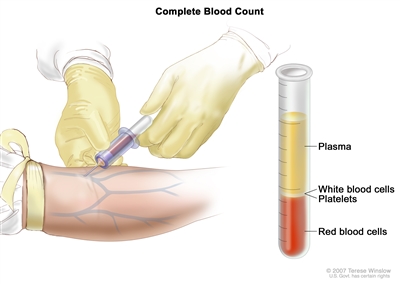
Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions. - Peripheral blood smear checks a sample of blood for blast cells, the number and kinds of white blood cells, the number of platelets, and changes in the shape of blood cells.
- Flow cytometry measures the number of cells in a sample, the percentage of live cells in a sample, and certain characteristics of the cells, such as size, shape, and the presence of tumor (or other) markers on the cell surface. The cells from a sample of a patient's blood, bone marrow, or other tissue are stained with a fluorescent dye, placed in a fluid, and then passed one at a time through a beam of light. The test results are based on how the cells that were stained with the fluorescent dye react to the beam of light. This test is used to help diagnose and manage certain types of cancers, such as leukemia and lymphoma.
-
Bone marrow aspiration and biopsy is the removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone. A pathologist views the bone marrow, blood, and bone under a microscope to look for signs of cancer.
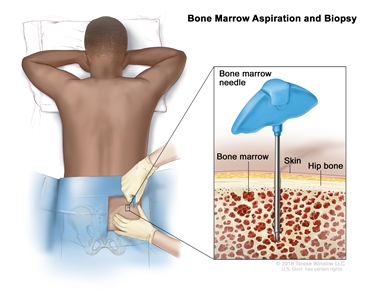
Bone marrow aspiration and biopsy. After a small area of skin is numbed, a long, hollow needle is inserted through the patient's skin and hip bone into the bone marrow. A sample of bone marrow and a small piece of bone are removed for examination under a microscope. - Tumor biopsy is the removal of cells or tissues from a lump using a needle. This may be done if the doctor suspects the leukemia cells may have formed a solid tumor called a myeloid sarcoma (also called a chloroma).
- Cytogenetic analysis checks the chromosomes of cells in a blood or bone marrow sample for changes, such as broken, missing, rearranged, or extra chromosomes. Changes in certain chromosomes may be a sign of cancer. Cytogenetic analysis is used to help diagnose cancer, plan treatment, or find out how well treatment is working. Other tests, such as fluorescence in situ hybridization (FISH), may also be done to look for certain changes in the chromosomes.
- Molecular testing checks for certain genes, proteins, or other molecules in a sample of blood or bone marrow. Molecular tests also check for certain changes in a gene or chromosome that may cause or affect the chance of developing AML. A molecular test may be used to help plan treatment, find out how well treatment is working, or make a prognosis.
- Immunophenotyping uses antibodies to identify cancer cells based on the types of antigens or markers on the surface of the cells. This test is used to help diagnose specific types of leukemia. For example, a cytochemistry study may test the cells in a sample of tissue using chemicals (dyes) to look for certain changes in the sample. A chemical may cause a color change in one type of leukemia cell but not in another type of leukemia cell.
- Reverse transcription–polymerase chain reaction test (RT-PCR) measures the amount of a genetic substance called mRNA made by a specific gene. An enzyme called reverse transcriptase is used to convert a specific piece of RNA into a matching piece of DNA, which can be amplified (made in large numbers) by another enzyme called DNA polymerase. The amplified DNA copies help tell whether a specific mRNA is being made by a gene. RT-PCR can be used to check the activation of certain genes that may indicate the presence of cancer cells. This test may be used to look for certain changes in a gene or chromosome, which may help diagnose cancer. This test is used to diagnose certain types of AML including acute promyelocytic leukemia (APL).
After AML has been diagnosed, tests are done to find out if the cancer has spread to other parts of the body.
The following tests and procedures may be used to determine if the leukemia has spread outside the blood and bone marrow:
-
Lumbar puncture is a procedure used to collect a sample of cerebrospinal fluid (CSF) from the spinal column. This is done by placing a needle between two bones in the spine and into the lining around the spinal cord to remove a sample of CSF. The sample of CSF is checked under a microscope for signs that leukemia cells have spread to the brain and spinal cord. This procedure is also called an LP or spinal tap.
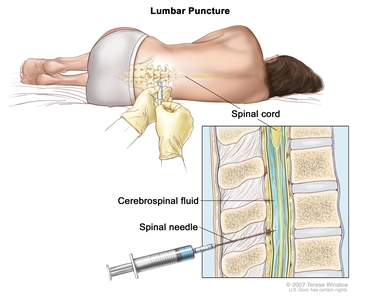
Lumbar puncture. A patient lies in a curled position on a table. After a small area on the lower back is numbed, a spinal needle (a long, thin needle) is inserted into the lower part of the spinal column to remove cerebrospinal fluid (CSF, shown in blue). The fluid may be sent to a laboratory for testing. - CT scan (CAT scan) uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, such as the abdomen. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Learn more about Computed Tomography (CT) Scans and Cancer.
Some people decide to get a second opinion.
You may want to get a second opinion to confirm your AML diagnosis and treatment plan. If you seek a second opinion, you will need to get medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the pathology report, slides, and scans. They may agree with the first doctor, suggest changes or another treatment approach, or provide more information about your cancer.
To learn more about choosing a doctor and getting a second opinion, visit Finding Cancer Care. You can contact NCI's Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor, hospital, or getting a second opinion. For questions you might want to ask at your appointments, visit Questions to Ask Your Doctor about Cancer.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis and treatment options for AML depend on:
- the person's age
- whether the leukemia has spread to the CNS
- whether the patient has a systemic infection at the time of diagnosis
- whether the patient has a very high white blood cell count at the time of diagnosis
- the subtype of AML
- whether the patient received chemotherapy or radiation therapy in the past to treat a different cancer
- whether there is a history of a blood disorder such as myelodysplastic syndrome
- whether the cancer has been treated before or recurred (come back)
It is important to treat AML right away. Older age at diagnosis may be linked to lower remission rates and more complications.
Stages of Acute Myeloid Leukemia
There is no standard staging system for acute myeloid leukemia (AML).
The extent or spread of cancer is usually described as stages. Instead of stages, AML treatment is based on one or more of the following:
- the subtype of AML
- whether the leukemia has spread outside the blood and bone marrow
- whether the leukemia is newly diagnosed, in remission, refractory, or recurrent
Newly diagnosed (untreated) AML
In untreated AML, the disease is newly diagnosed. It has not been treated except to relieve signs and symptoms such as fever, bleeding, or pain, and the following are true:
- The complete blood count (CBC) is abnormal.
- At least 20% of the cells in the bone marrow are blasts (leukemia cells) or there are certain gene changes.
- There are signs or symptoms of leukemia.
AML in remission
In AML in remission, the disease has been treated and the following are true:
- The CBC is normal.
- Less than 5% of the cells in the bone marrow are blasts (leukemia cells).
- There are no signs or symptoms of leukemia in the brain and spinal cord or elsewhere in the body.
Refractory or recurrent AML
After treatment with chemotherapy, some people with newly diagnosed AML will not go into remission. This is called refractory cancer. In contrast, recurrent AML is cancer that has recurred (come back) after remission. The AML may come back in the blood or bone marrow.
Learn more in Recurrent Cancer: When Cancer Comes Back. Information to help you cope and talk with your health care team can be found in the booklet When Cancer Returns.
Treatment Option Overview
There are different types of treatment for people with acute myeloid leukemia (AML).
Different types of treatments are available for people with AML. You and your cancer care team will work together to decide your treatment plan, which may include more than one type of treatment. Many factors will be considered, such as the phase of the cancer, your overall health, and your preferences. Your plan will include information about your cancer, the goals of treatment, your treatment options and the possible side effects, and the expected length of treatment.
Talking with your cancer care team before treatment begins about what to expect will be helpful. You'll want to learn what you need to do before treatment begins, how you'll feel while going through it, and what kind of help you will need. Learn more at Questions to Ask Your Doctor about Treatment.
The treatment of AML usually has two phases.
There are two treatment phases of AML:
- Remission induction therapy is the first phase of treatment. The goal is to kill the leukemia cells in the blood and bone marrow. This puts the leukemia into remission.
- Consolidation therapy is the second phase of treatment. It begins after the leukemia is in remission. The goal of consolidation therapy is to kill any remaining leukemia cells that may not be active but could begin to regrow and cause a relapse. This phase is also called remission continuation therapy.
Patients receive supportive care for side effects of treatment.
Patients must be closely monitored during treatment of AML. Myelosuppression, a condition which results in fewer red blood cells, white blood cells, and platelets, is a side effect of both AML and treatment with chemotherapy. Supportive care during remission induction therapy may include:
- red blood cell and platelet transfusions to replace blood cells destroyed by the cancer or its treatment
- antibiotics and antifungals to prevent or treat infections
The following types of treatment are used:
Chemotherapy
Chemotherapy (also called chemo) uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. The way the chemotherapy is given depends on the subtype of AML being treated and whether the leukemia cells have spread to the central nervous system (CNS; brain and spinal cord).
Systemic chemotherapy is when chemotherapy drugs are taken by mouth or injected into a vein or muscle. When given this way, the drugs enter the bloodstream and can reach cancer cells throughout the body.
Systemic chemotherapy drugs used to treat AML include:
- azacitidine
- cytarabine
- daunorubicin
- daunorubicin and cytarabine
- decitabine
- idarubicin
- midostaurin
- mitoxantrone
Combinations of these drugs may be used. Other chemotherapy drugs not listed here may also be used.
Intrathecal chemotherapy may be used to treat AML that has spread to the CNS (brain and spinal cord). Intrathecal chemotherapy is a method of placing chemotherapy directly into the cerebrospinal fluid, which is the fluid that surrounds the brain and spinal cord. This approach is used because the blood-brain barrier, a protective layer around the brain, can prevent chemotherapy drugs given by mouth or into a vein from reaching the CNS.
Cytarabine and methotrexate are two chemotherapy drugs given as intrathecal chemotherapy to treat AML. These drugs can also be given systemically.
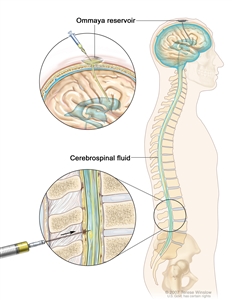
Intrathecal chemotherapy. Anticancer drugs are injected into the intrathecal space, which is the space that holds the cerebrospinal fluid (CSF, shown in blue). There are two different ways to do this. One way, shown in the top part of the figure, is to inject the drugs into an Ommaya reservoir (a dome-shaped container that is placed under the scalp during surgery; it holds the drugs as they flow through a small tube into the brain). The other way, shown in the bottom part of the figure, is to inject the drugs directly into the CSF in the lower part of the spinal column, after a small area on the lower back is numbed.
Learn more about how chemotherapy works, how it is given, common side effects, and more at Chemotherapy to Treat Cancer and Chemotherapy and You: Support for People With Cancer.
Radiation therapy
Radiation therapy uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. AML is sometimes treated with external radiation therapy. This type of radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. Total-body irradiation sends radiation toward the whole body. It is a type of external radiation that may be used to prepare the body for a stem cell transplant when the leukemia has recurred.
Learn more about External Beam Radiation Therapy for Cancer and Radiation Therapy Side Effects.
Chemotherapy with stem cell transplant
High doses of chemotherapy are given to kill cancer cells. Healthy cells, including blood-forming cells, are also destroyed by the cancer treatment. Stem cell transplant is a treatment to replace the blood-forming cells. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient or a donor and are frozen and stored. After the patient completes chemotherapy and/or total-body irradiation, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body's blood cells.
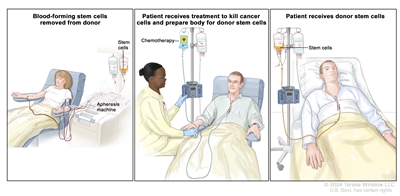
Donor stem cell transplant. (Step 1): Four to five days before donor stem cell collection, the donor receives a medicine to increase the number of stem cells circulating through their bloodstream (not shown). The blood-forming stem cells are then collected from the donor through a large vein in their arm. The blood flows through an apheresis machine that removes the stem cells. The rest of the blood is returned to the donor through a vein in their other arm. (Step 2): The patient receives chemotherapy to kill cancer cells and prepare their body for the donor stem cells. The patient may also receive radiation therapy (not shown). (Step 3): The patient receives an infusion of the donor stem cells.
Learn more about Stem Cell Transplants in Cancer Treatment.
Targeted therapy
Targeted therapy uses drugs or other substances to identify and attack specific cancer cells. Your doctor may suggest biomarker tests to help predict your response to certain targeted therapy drugs. Learn more about Biomarker Testing for Cancer Treatment.
Targeted therapies used to treat AML include:
- gemtuzumab ozogamicin
- midostaurin
- quizartinib
- revumenib
Less-intensive targeted therapies in people who are unable or unwilling to receive other treatments include:
- enasidenib
- gilteritinib
- glasdegib
- ivosidenib
- venetoclax
Learn more about Targeted Therapy to Treat Cancer.
Other drug therapy
Arsenic trioxide and all-trans retinoic acid (ATRA) are anticancer drugs that kill leukemia cells, stop the leukemia cells from dividing, or help the leukemia cells mature into white blood cells. These drugs are used in the treatment of a subtype of AML called acute promyelocytic leukemia.
New types of treatment are being tested in clinical trials.
For some people, joining a clinical trial may be an option. There are different types of clinical trials for people with cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Clinical Trials Information for Patients and Caregivers.
Treatment for acute myeloid leukemia may cause side effects.
For information about side effects caused by treatment for cancer, visit our Side Effects page.
Follow-up care may be needed.
As you go through treatment, you will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
Treatment of Untreated Acute Myeloid Leukemia
Standard treatment of untreated acute myeloid leukemia (AML) during the remission induction phase depends on the subtype of AML and may include:
- combination chemotherapy that includes cytarabine
- combination chemotherapy with targeted therapy (midostaurin or quizartinib), for people whose AML has a mutation in the FLT3 gene
- combination chemotherapy with the targeted therapy drug gemtuzumab ozogamicin
- intrathecal chemotherapy (cytarabine or methotrexate), for central nervous system (CNS) leukemia
- supportive care
For older adults or people who are unable or unwilling to receive intensive chemotherapy, the following may be continued as long as the person benefits or until toxic effects occur:
- targeted therapy (enasidenib, gilteritinib, glasdegib, ivosidenib, or venetoclax)
- low-dose chemotherapy (azacitidine, low-dose cytarabine, or decitabine)
- targeted therapy with low-dose chemotherapy
- intrathecal chemotherapy, for CNS leukemia
- supportive care
Learn more about these treatments in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Acute Myeloid Leukemia in Remission
Treatment of acute myeloid leukemia (AML) during the remission phase depends on the subtype of AML and may include:
- combination chemotherapy that includes cytarabine
- maintenance therapy with midostaurin, for people whose AML has a mutation in the FLT3 gene
- maintenance therapy with chemotherapy
- high-dose chemotherapy and stem cell transplant using the patient's stem cells
- high-dose chemotherapy, with or without radiation therapy, or reduced-intensity therapy, followed by a stem cell transplant using donor stem cells
Learn more about these treatments in Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Refractory or Recurrent Acute Myeloid Leukemia
There is no standard treatment for refractory or recurrent acute myeloid leukemia (AML). Treatment depends on the subtype of AML and may include:
- combination chemotherapy
- targeted therapy with enasidenib, gemtuzumab ozogamicin, gilteritinib, ivosidenib, or revumenib
- stem cell transplant using donor stem cells
Learn more about these treatments in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Acute Promyelocytic Leukemia
Treatment of newly diagnosed acute promyelocytic leukemia (APL) may include:
- all-trans retinoic acid (ATRA) plus arsenic trioxide (ATO), for low-risk to intermediate-risk disease
- ATRA plus combination chemotherapy, followed by ATO, for high-risk disease
Learn more about these treatments in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Recurrent Acute Promyelocytic Leukemia
Treatment of recurrent acute promyelocytic leukemia (APL) may include:
- arsenic trioxide (ATO) with or without chemotherapy
- stem cell transplant using the patient's stem cells or donor stem cells
Learn more about these treatments in the Treatment Option Overview.
To Learn More About Leukemia
For more information from the National Cancer Institute about leukemia, visit the Leukemia Home Page.
For general cancer information and other resources from the National Cancer Institute, visit:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of adult acute myeloid leukemia. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Acute Myeloid Leukemia Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/leukemia/patient/adult-aml-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389377]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2025-04-14
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.


