Hodgkin Lymphoma Treatment (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Hodgkin Lymphoma
Hodgkin lymphoma is a disease in which malignant (cancer) cells form in the lymph system.
Hodgkin lymphoma is a type of cancer that develops in the lymph system. The lymph system is part of the immune system. It helps protect the body from infection and disease.
The lymph system is made up of:
- Lymph: Colorless, watery fluid that travels through the lymph vessels and carries T and B lymphocytes. Lymphocytes are a type of white blood cell.
- Lymph vessels: A network of thin tubes that collect lymph from different parts of the body and return it to the bloodstream.
- Lymph nodes: Small, bean-shaped structures that filter lymph and store white blood cells that help fight infection and disease. Lymph nodes are found along a network of lymph vessels throughout the body. Groups of lymph nodes are found in the mediastinum (the area between the lungs), neck, underarm, abdomen, pelvis, and groin. Hodgkin lymphoma most commonly forms in the lymph nodes above the diaphragm and often in the lymph nodes in the mediastinum.
- Spleen: An organ that makes lymphocytes, stores red blood cells and lymphocytes, filters the blood, and destroys old blood cells. The spleen is on the left side of the abdomen near the stomach.
- Thymus: An organ in which T lymphocytes mature and multiply. The thymus is in the chest behind the breastbone.
- Bone marrow: The soft, spongy tissue in the center of certain bones, such as the hip bone and breastbone. White blood cells, red blood cells, and platelets are made in the bone marrow.
- Tonsils: Two small masses of lymph tissue at the back of the throat. There is one tonsil on each side of the throat. Hodgkin lymphoma rarely forms in the tonsils.

The lymph system is part of the body's immune system and is made up of tissues and organs that help protect the body from infection and disease. These include the tonsils, adenoids (not shown), thymus, spleen, bone marrow, lymph vessels, and lymph nodes. Lymph tissue is also found in many other parts of the body, including the small intestine.
Lymph tissue is also found in other parts of the body, such as the lining of the digestive tract, bronchus, and skin.
There are two general types of lymphoma: Hodgkin lymphoma and non-Hodgkin lymphoma. This summary is about the treatment of Hodgkin lymphoma in adults, including during pregnancy.
The two main types of Hodgkin lymphoma are classic and nodular lymphocyte-predominant.
Most Hodgkin lymphomas are the classic type. When a sample of lymph node tissue is looked at under a microscope, Hodgkin lymphoma cancer cells, called Reed-Sternberg cells, may be seen. The classic type is broken down into the following four subtypes:
- Nodular sclerosing Hodgkin lymphoma.
- Mixed cellularity Hodgkin lymphoma.
- Lymphocyte-depleted Hodgkin lymphoma.
- Lymphocyte-rich classic Hodgkin lymphoma.
Nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL) is rare and tends to grow slower than classic Hodgkin lymphoma. NLPHL often presents as a swollen lymph node in the neck, chest, armpit, or groin. Most people do not have any other signs or symptoms of cancer at diagnosis. Treatment is often different from classic Hodgkin lymphoma.
Being in early or late adulthood, being male, past Epstein-Barr infection, and a family history of Hodgkin lymphoma can increase the risk of Hodgkin lymphoma.
Anything that increases a person's chance of getting a disease is called a risk factor. Not every person with one or more of these risk factors will develop Hodgkin lymphoma, and it can develop in people who don't have any known risk factors. Talk with your doctor if you think you may be at risk. Risk factors for Hodgkin lymphoma include:
- Age. Hodgkin lymphoma is most common in early adulthood (age 20–39 years) and in late adulthood (age 65 years and older).
- Being male. The risk of Hodgkin lymphoma is slightly higher in males than in females.
- Past Epstein-Barr virus infection. Having an infection with the Epstein-Barr virus in the teenage years or early childhood increases the risk of Hodgkin lymphoma.
- A family history of Hodgkin lymphoma. Having a parent, brother, or sister with Hodgkin lymphoma increases the risk of developing Hodgkin lymphoma.
Signs and symptoms of Hodgkin lymphoma include swollen lymph nodes, fever, drenching night sweats, weight loss, and fatigue.
These and other signs and symptoms may be caused by Hodgkin lymphoma or by other conditions. Check with your doctor if you have any of the following symptoms that do not go away:
- Painless, swollen lymph nodes in the neck, underarm, or groin.
- Fever for no known reason.
- Drenching night sweats.
- Weight loss for no known reason in the past 6 months.
- Pruritus (itchy skin), especially after bathing or drinking alcohol.
- Feeling very tired.
Tests that examine the lymph system and other parts of the body are used to help diagnose and stage Hodgkin lymphoma.
In addition to asking about your personal and family health history and doing a physical exam, your doctor may perform the following tests and procedures:
-
Complete blood count (CBC): A procedure in which a sample of blood is drawn and checked for:
- The number of red blood cells, white blood cells, and platelets.
- The amount of hemoglobin (the protein that carries oxygen) in the red blood cells.
- The portion of the sample made up of red blood cells.
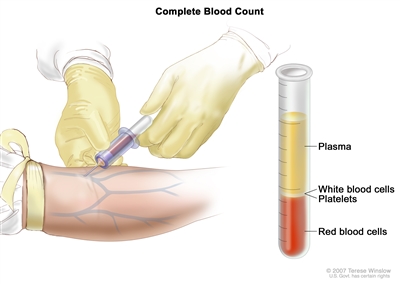
Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions. - Blood chemistry studies: A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- LDH test: A procedure in which a blood sample is checked to measure the amount of lactic dehydrogenase (LDH). An increased amount of LDH in the blood may be a sign of tissue damage, lymphoma, or other diseases.
- Hepatitis B and hepatitis C test: A procedure in which a sample of blood is checked to measure the amounts of hepatitis B virus-specific antigens and/or antibodies and the amounts of hepatitis C virus-specific antibodies. These antigens or antibodies are called markers. Different markers or combinations of markers are used to determine whether a patient has a hepatitis B or C infection, has had a prior infection or vaccination, or is susceptible to infection. Knowing whether a patient has hepatitis B or C may help plan treatment.
- HIV test: A test to measure the level of HIV antibodies in a sample of blood. Antibodies are made by the body when it is invaded by a foreign substance. A high level of HIV antibodies may mean the body has been infected with HIV. Knowing whether a patient has HIV may help plan treatment.
- Sedimentation rate: A procedure in which a sample of blood is drawn and checked for the rate at which the red blood cells settle to the bottom of the test tube. The sedimentation rate is a measure of how much inflammation is in the body. A higher than normal sedimentation rate may be a sign of lymphoma or another condition. Also called erythrocyte sedimentation rate, sed rate, or ESR.
-
PET-CT scan: A procedure that combines the pictures from a positron emission tomography (PET) scan and a computed tomography (CT) scan. The PET and CT scans are done at the same time on the same machine. The pictures from both scans are combined to make a more detailed picture than either test would make by itself. A PET-CT scan may be used to help diagnose disease, such as cancer, determine stage, plan treatment, or find out how well treatment is working. A PET-magnetic resonance imaging (MRI) scan may be done in place of a PET-CT scan and uses a lower dose of radiation.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, such as the neck, chest, abdomen, pelvis, and lymph nodes, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. If a PET-CT scan is not available, a CT scan alone may be done.
- PET scan (positron emission tomography scan): A PET scan is a procedure to find cancer cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Cancer cells show up brighter in the picture because they are more active and take up more glucose than normal cells do.
-
Lymph node biopsy: The removal of all or part of a lymph node. A pathologist views the tissue under a microscope to look for cancer cells called Reed-Sternberg cells. Reed-Sternberg cells are common in classic Hodgkin lymphoma.
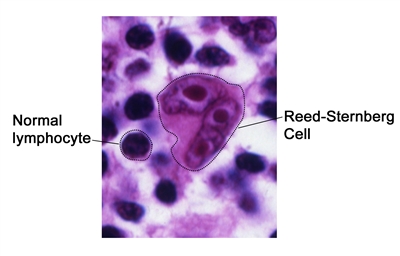
Reed-Sternberg cell. Reed-Sternberg cells are large, abnormal lymphocytes (a type of white blood cell) that may contain more than one nucleus. These cells are found in people with Hodgkin lymphoma. Reed-Sternberg cells are also called Hodgkin and Reed-Sternberg cells.One of the following types of biopsies may be done:
- Excisional biopsy: The removal of an entire lymph node.
- Incisional biopsy: The removal of part of a lymph node.
- Core biopsy: The removal of tissue from a lymph node using a wide needle.
Other areas of the body, such as the liver, lung, bone, bone marrow, and brain, may also have a sample of tissue removed and checked by a pathologist for signs of cancer.
The following test may be done on tissue that was removed:
- Immunophenotyping: A laboratory test that uses antibodies to identify cancer cells based on the types of antigens or markers on the surface of the cells. This test is used to help diagnose specific types of lymphoma.
For pregnant women with Hodgkin lymphoma, imaging tests that protect the fetus from the harms of radiation are used. These include:
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI). In women who are pregnant, contrast dye is not used during the procedure.
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis and treatment options depend on:
- The patient's signs and symptoms, including whether or not they have B symptoms (fever for no known reason, weight loss for no known reason, or drenching night sweats).
- The stage of the cancer (the size of the cancer tumors and whether the cancer has spread to the abdomen or more than one group of lymph nodes).
- The type of Hodgkin lymphoma.
- Blood test results.
- The patient's age, sex, and general health.
- Whether the cancer is newly diagnosed, continues to grow during treatment, or has come back after treatment.
For Hodgkin lymphoma during pregnancy, treatment options also depend on:
- The wishes of the patient.
- The age of the fetus.
Hodgkin lymphoma can usually be cured if found and treated early.
Stages of Hodgkin Lymphoma
After Hodgkin lymphoma has been diagnosed, tests are done to find out if cancer cells have spread within the lymph system or to other parts of the body.
The process used to find out if cancer has spread within the lymph system or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage to plan treatment. The results of the tests and procedures done to diagnose and stage Hodgkin lymphoma are used to help make decisions about treatment.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
The following stages are used for Hodgkin lymphoma:
Stage I

Stage I adult lymphoma. Cancer is found in one or more lymph nodes in a group of lymph nodes or, in rare cases, cancer is found in the Waldeyer's ring, thymus, or spleen. In stage IE (not shown), cancer has spread to one area outside the lymph system.
Stage I Hodgkin lymphoma is divided into stages I and IE.
- In stage I, cancer is found in one of the following places in the lymph system:
- One or more lymph nodes in a group of lymph nodes.
- Waldeyer's ring.
- Thymus.
- Spleen.
- In stage IE, cancer is found in one area outside the lymph system.
Stage II
Stage II Hodgkin lymphoma is divided into stages II and IIE.
- In stage II, cancer is found in two or more groups of lymph nodes that are either above the diaphragm or below the diaphragm.
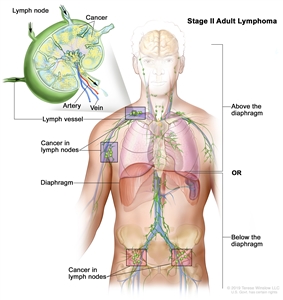
Stage II adult lymphoma. Cancer is found in two or more groups of lymph nodes that are either above the diaphragm or below the diaphragm. - In stage IIE, cancer has spread from a group of lymph nodes to a nearby area that is outside the lymph system. Cancer may have spread to other lymph node groups on the same side of the diaphragm.
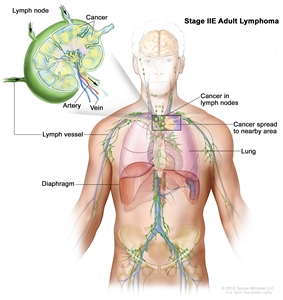
Stage IIE adult lymphoma. Cancer has spread from a group of lymph nodes to a nearby area that is outside the lymph system. Cancer may have spread to other lymph node groups on the same side of the diaphragm.
In stage II, the term bulky disease refers to a larger tumor mass. The size of the tumor mass that is referred to as bulky disease varies based on the type of lymphoma.
Stage III
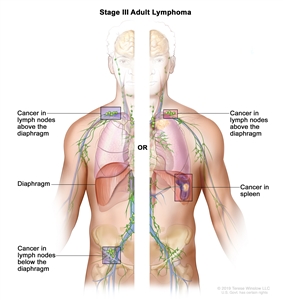
Stage III adult lymphoma. Cancer is found in groups of lymph nodes both above and below the diaphragm; or in a group of lymph nodes above the diaphragm and in the spleen.
In stage III Hodgkin lymphoma, cancer is found:
- in groups of lymph nodes both above and below the diaphragm; or
- in lymph nodes above the diaphragm and in the spleen.
Stage IV
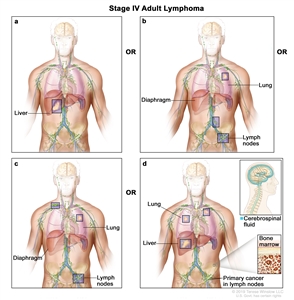
Stage IV adult lymphoma. Cancer (a) has spread throughout one or more organs outside the lymph system; or (b) is found in two or more groups of lymph nodes that are either above the diaphragm or below the diaphragm and in one organ that is outside the lymph system and not near the affected lymph nodes; or (c) is found in groups of lymph nodes above the diaphragm and below the diaphragm and in any organ that is outside the lymph system; or (d) is found in the liver, bone marrow, more than one place in the lung, or cerebrospinal fluid (CSF). The cancer has not spread directly into the liver, bone marrow, lung, or CSF from nearby lymph nodes.
In stage IV Hodgkin lymphoma, cancer:
- has spread throughout one or more organs outside the lymph system; or
- is found in two or more groups of lymph nodes that are either above the diaphragm or below the diaphragm and in one organ that is outside the lymph system and not near the affected lymph nodes; or
- is found in groups of lymph nodes both above and below the diaphragm and in any organ that is outside the lymph system; or
- is found in the liver, bone marrow, more than one place in the lung, or cerebrospinal fluid (CSF). The cancer has not spread directly into the liver, bone marrow, lung, or CSF from nearby lymph nodes.
Hodgkin lymphoma may be grouped for treatment as follows:
Early Favorable
Early favorable Hodgkin lymphoma is stage I or stage II, without risk factors that increase the chance that the cancer will come back after it is treated.
Early Unfavorable
Early unfavorable Hodgkin lymphoma is stage I or stage II with one or more of the following risk factors that increase the chance that the cancer will come back after it is treated:
- Having a tumor in the chest that is larger than 1/3 of the width of the chest or is at least 10 centimeters.
- Having cancer in an organ other than the lymph nodes.
- Having a high sedimentation rate (in a sample of blood, the red blood cells settle to the bottom of the test tube more quickly than normal).
- Having three or more lymph nodes with cancer.
- Having B symptoms (fever for no known reason, weight loss for no known reason, or drenching night sweats).
Advanced
Advanced Hodgkin lymphoma is stage III or stage IV. Advanced favorable Hodgkin lymphoma means that the patient has 0–3 of the risk factors below. Advanced unfavorable Hodgkin lymphoma means that the patient has 4 or more of the risk factors below. The more risk factors a patient has, the more likely it is that the cancer will come back after it is treated:
- Having a low blood albumin level (below 4).
- Having a low hemoglobin level (below 10.5).
- Being male.
- Being aged 45 years or older.
- Having stage IV disease.
- Having a high white blood cell count (15,000 or higher).
- Having a low lymphocyte count (below 600 or less than 8% of the white blood cell count).
Hodgkin lymphoma can recur (come back) after it has been treated.
The cancer may come back in the lymph system or in other parts of the body.
Treatment Option Overview
There are different types of treatment for patients with Hodgkin lymphoma.
Different types of treatment are available for patients with Hodgkin lymphoma. Some treatments are standard (currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
For pregnant women with Hodgkin lymphoma, treatment is carefully chosen to protect the fetus. Treatment decisions are based on the mother's wishes, the stage of the Hodgkin lymphoma, and the trimester of the pregnancy. The treatment plan may change as the signs and symptoms, cancer, and pregnancy change. Choosing the most appropriate cancer treatment is a decision that ideally involves the patient, family, and health care team.
Patients with Hodgkin lymphoma should have their treatment planned by a team of health care providers with expertise in treating lymphomas.
Treatment will be overseen by a medical oncologist, a doctor who specializes in treating cancer. The medical oncologist may refer you to other health care providers who have experience and expertise in treating Hodgkin lymphoma and who specialize in certain areas of medicine. These may include the following specialists:
- Radiation oncologist.
- Rehabilitation specialist.
- Hematologist.
- Fertility specialist.
- Other oncology specialists.
Treatment for Hodgkin lymphoma may cause side effects.
To learn more about side effects that begin during treatment for cancer, visit Side Effects.
Side effects from cancer treatment that begin after treatment and continue for months or years are called late effects. Treatment with chemotherapy and/or radiation therapy for Hodgkin lymphoma may increase the risk of second cancers and other health problems for many months or years after treatment. These late effects depend on the type of treatment and the patient's age when treated, and may include:
- Second cancers.
- Solid tumors, such as mesothelioma and cancer of the lung, breast, thyroid, bone, soft tissue, stomach, esophagus, colon, rectum, cervix, and head and neck.
- Acute myelogenous leukemia.
- Infertility.
- Hypothyroidism (too little thyroid hormone in the blood).
- Heart disease, such as heart attack.
- Lung problems, such as trouble breathing.
- Avascular necrosis of bone (death of bone cells caused by lack of blood flow).
- Severe infection.
- Chronic fatigue.
- Cognitive impairment.
Regular follow-up by doctors who are experts in finding and treating late effects is important for the long-term health of patients treated for Hodgkin lymphoma.
The following types of treatment are used:
Chemotherapy
Chemotherapy is a cancer treatment that uses one or more drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. Cancer treatment using more than one chemotherapy drug is called combination chemotherapy. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy).
When a pregnant woman is treated with chemotherapy for Hodgkin lymphoma, it isn't possible to protect the fetus from being exposed to the chemotherapy. Some chemotherapy regimens may cause birth defects if given in the first trimester. Vinblastine is an anticancer drug that has not been linked with birth defects when given in the second or third trimester of pregnancy.
For more information, see Drugs Approved for Hodgkin Lymphoma.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. Sometimes total-body irradiation is given before a stem cell transplant.
Proton beam radiation therapy is a type of high-energy, external radiation therapy that uses streams of protons (tiny particles with a positive charge) to kill tumor cells. This type of treatment can lower the amount of radiation damage to healthy tissue near a tumor such as the heart or breast.
External radiation therapy is used to treat Hodgkin lymphoma and may also be used as palliative therapy to relieve symptoms and improve quality of life.
For a pregnant woman with Hodgkin lymphoma, radiation therapy should be postponed until after delivery, if possible, to avoid any risk of radiation exposure during fetal development. If treatment is needed right away, the woman may decide to continue the pregnancy and receive radiation therapy. A lead shield is used to cover the pregnant woman's abdomen to help protect the fetus from radiation as much as possible.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells.
- Monoclonal antibodies: Monoclonal antibodies are immune system proteins made in the laboratory to treat many diseases, including cancer. As a cancer treatment, these antibodies can attach to a specific target on cancer cells or other cells that may help cancer cells grow. The antibodies are able to then kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells. Brentuximab vedotin and rituximab are monoclonal antibodies used to treat Hodgkin lymphoma.monoclonal antibodies: how monoclonal antibodies treat cancerHow do monoclonal antibodies work to treat cancer? This video shows how monoclonal antibodies, such as trastuzumab, pembrolizumab, and rituximab, block molecules cancer cells need to grow, flag cancer cells for destruction by the body's immune system, or deliver harmful substances to cancer cells.
For more information, see Drugs Approved for Hodgkin Lymphoma.
Immunotherapy
Immunotherapy is a treatment that uses the patient's immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body's natural defenses against cancer.
- PD-1 and PD-L1 inhibitor therapy: PD-1 is a protein on the surface of T cells that helps keep the body's immune responses in check. PD-L1 is a protein found on some types of cancer cells. When PD-1 attaches to PD-L1, it stops the T cell from killing the cancer cell. PD-1 and PD-L1 inhibitors keep PD-1 and PD-L1 proteins from attaching to each other. This allows the T cells to kill cancer cells. Pembrolizumab and nivolumab are types of PD-1 inhibitors used to treat Hodgkin lymphoma that has recurred (come back).
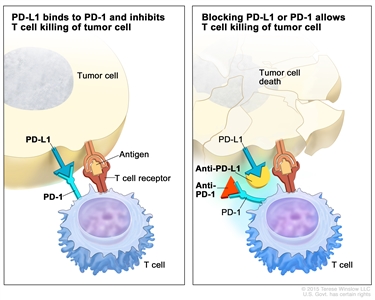
Immune checkpoint inhibitor. Checkpoint proteins, such as PD-L1 on tumor cells and PD-1 on T cells, help keep immune responses in check. The binding of PD-L1 to PD-1 keeps T cells from killing tumor cells in the body (left panel). Blocking the binding of PD-L1 to PD-1 with an immune checkpoint inhibitor (anti-PD-L1 or anti-PD-1) allows the T cells to kill tumor cells (right panel).
For more information, see Drugs Approved for Hodgkin Lymphoma.
Chemotherapy with stem cell transplant
High doses of chemotherapy are given to kill cancer cells. Healthy cells, including blood-forming cells, are also destroyed by the cancer treatment. Stem cell transplant is a treatment to replace the blood-forming cells. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient or a donor and are frozen and stored. After the patient completes chemotherapy and radiation therapy, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body's blood cells.
For patients with nodular lymphocyte–predominant Hodgkin lymphoma (NLPHL), treatment options also include:
Watchful waiting
Watchful waiting is closely monitoring a patient's condition without giving any treatment until signs or symptoms appear or change.
Active surveillance
Active surveillance is a treatment plan that involves closely watching a patient's condition but not giving any treatment unless there are changes in test results that show the condition is getting worse. During active surveillance, certain exams and tests are done on a regular schedule.
For pregnant patients with Hodgkin lymphoma, treatment options also include:
Watchful waiting
Watchful waiting is closely monitoring a patient's without giving any treatment unless signs or symptoms appear or change. Labor may be induced when the fetus is 32 to 36 weeks so that the mother can begin treatment.
Steroid therapy
Steroids are hormones made naturally in the body by the adrenal glands and by reproductive organs. Some types of steroids are made in a laboratory. Certain steroid drugs have been found to help chemotherapy work better and help stop the growth of cancer cells. When an early delivery is likely, steroids can also help the lungs of the fetus develop faster than normal. This gives babies who are born early a better chance of survival.
For more information, see Drugs Approved for Hodgkin Lymphoma.
New types of treatment are being tested in clinical trials.
Information about clinical trials is available from the NCI website.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI's clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up care may be needed.
As you go through treatment, you will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
Treatment of Early Favorable Classic Hodgkin Lymphoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of early favorable classic Hodgkin lymphoma in adults may include:
- Combination chemotherapy with or without radiation therapy to the areas of the body with cancer.
- Radiation therapy alone in patients who cannot be treated with combination chemotherapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Early Unfavorable Classic Hodgkin Lymphoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of early unfavorable classic Hodgkin lymphoma in adults may include:
- Combination chemotherapy with or without radiation therapy to the areas of the body with cancer.
- Targeted therapy with a monoclonal antibody (brentuximab vedotin) and combination chemotherapy with or without radiation therapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Advanced Classic Hodgkin Lymphoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of advanced classic Hodgkin lymphoma in adults may include:
- Combination chemotherapy with or without immunotherapy (nivolumab) or targeted therapy (brentuximab vedotin).
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Recurrent Classic Hodgkin Lymphoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of recurrent classic Hodgkin lymphoma in adults may include:
- Immunotherapy with an immune checkpoint inhibitor (pembrolizumab or nivolumab) with or without combination chemotherapy. This may be followed by stem cell transplant.
- Targeted therapy with a monoclonal antibody (brentuximab vedotin) with or without immunotherapy with an immune checkpoint inhibitor (nivolumab).
- Combination chemotherapy with radiation therapy to the areas of the body with cancer for patients older than 60 years.
- Radiation therapy with or without chemotherapy, for patients whose cancer came back only in the lymph nodes.
- Immunotherapy as palliative therapy to relieve symptoms and improve quality of life.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Nodular Lymphocyte–Predominant Hodgkin Lymphoma (NLPHL)
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of NLPHL in adults may include:
- Watchful waiting or active surveillance.
- Radiation therapy to the areas of the body with cancer, for patients with early-stage NLPHL.
- Chemotherapy, for patients with advanced-stage NLPHL.
- Targeted therapy with a monoclonal antibody (rituximab).
Treatment of Hodgkin Lymphoma During Pregnancy
For information about the treatments listed below, see the Treatment Option Overview section.
Hodgkin Lymphoma During the First Trimester of Pregnancy
When Hodgkin lymphoma is diagnosed in the first trimester of pregnancy, it does not necessarily mean that the woman will be advised to end the pregnancy. Each woman's treatment will depend on the stage of the lymphoma, how fast it is growing, and her wishes. Treatment of Hodgkin lymphoma during the first trimester of pregnancy may include:
- Watchful waiting when the cancer is above the diaphragm and is slow-growing. Labor may be induced early so the mother can begin treatment.
- Radiation therapy when the cancer is above the diaphragm. A lead shield is used to protect the fetus from the radiation as much as possible.
- Chemotherapy using one or more drugs.
Hodgkin Lymphoma During the Second or Third Trimester of Pregnancy
When Hodgkin lymphoma is diagnosed in the second half of pregnancy, most women can delay treatment until after delivery. Treatment of Hodgkin lymphoma during the second or third trimester of pregnancy may include:
- Watchful waiting, with plans to induce labor when the fetus is 32 to 36 weeks.
- Radiation therapy to relieve breathing problems caused by a large tumor in the chest.
- Combination chemotherapy using one or more drugs.
- Steroid therapy.
To Learn More About Hodgkin Lymphoma
For more information from the National Cancer Institute about Hodgkin lymphoma, visit:
- Lymphoma Home Page
- Drugs Approved for Hodgkin Lymphoma
- Targeted Therapy to Treat Cancer
- Immunotherapy to Treat Cancer
For general cancer information and other resources from the National Cancer Institute, visit:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of adult Hodgkin lymphoma. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Hodgkin Lymphoma Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/lymphoma/patient/adult-hodgkin-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389245]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2025-02-27
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.


