Langerhans Cell Histiocytosis Treatment (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Langerhans Cell Histiocytosis (LCH)
Langerhans cell histiocytosis is a rare disorder that can damage tissue or cause lesions to form in one or more places in the body.
Langerhans cell histiocytosis (LCH) is a rare disease that begins in LCH cells. LCH cells are a type of dendritic cell that normally helps the body fight infection. Sometimes mutations (changes) develop in genes that control how dendritic cells function. These include mutations of the BRAF, MAP2K1, RAS, and ARAF genes. These mutations may cause too many LCH cells to grow and build up in certain parts of the body, where they can damage tissue or form lesions.
It is not known whether LCH is a form of cancer or a cancer-like disease.
Doctors who treat cancer also treat LCH, and sometimes they use cancer therapies to treat this disease. For more information, see the sections on the treatment of LCH in children and the treatment of LCH in adults.
Family history of cancer or having a parent who was exposed to certain chemicals may increase the risk of LCH.
Anything that increases a person's risk of getting a disease is called a risk factor. Not every child with one or more of these risk factors will develop LCH, and it will develop in some children who don't have any known risk factors. Talk with your doctor if you think you may be at risk.
Risk factors for LCH may include the following:
- Having a parent who was exposed to certain solvents.
- Having a parent who was exposed to metal, granite, or wood dust in the workplace.
- Having a family history of cancer or LCH.
- Having a personal history or family history of thyroid disease.
- Having infections as a newborn.
- Smoking, especially in young adults.
- Being Hispanic.
- Not being vaccinated as a child.
The signs and symptoms of LCH depend on where it is in the body.
These and other signs and symptoms may be caused by LCH or by other conditions. Check with your doctor if you or your child have any of the following:
Bone
Signs or symptoms of LCH that affects the bone may include:
- Swelling or a lump over a bone, such as the skull, jawbone, ribs, pelvis, spine, thigh bone, upper arm bone, elbow, eye socket, or bones around the ear.
- Pain where there is swelling or a lump over a bone.
Children with LCH lesions in bones around the ears or eyes have a high risk of diabetes insipidus and other central nervous system diseases.
Skin and nails
LCH in infants may affect the skin only. In some cases, skin-only LCH may get worse over weeks or months and become a form called high-risk multisystem LCH.
In infants, signs or symptoms of LCH that affects the skin may include:
- Flaking of the scalp that may look like "cradle cap."
- Flaking in the creases of the body, such as the inner elbow or perineum.
- Raised skin rash with brown or purple areas that occur anywhere on the body.
In children and adults, signs or symptoms of LCH that affects the skin and nails may include:
- Flaking of the scalp that may look like dandruff.
- Raised skin rash with red, brown, or crusted areas that may be itchy or painful. The rash can occur in the groin area or on the abdomen, back, or chest.
- Bumps or ulcers on the scalp.
- Ulcers behind the ears, under the breasts, or in the groin area.
- Fingernails that fall off or have discolored grooves that run across the nail.
Mouth
Signs or symptoms of LCH that affects the mouth may include:
- Swollen gums.
- Sores on the roof of the mouth, inside the cheeks, or on the tongue or lips.
- Teeth that become uneven or fall out.
Lymph nodes and thymus
Signs or symptoms of LCH that affects the lymph nodes or thymus may include:
- Swollen lymph nodes.
- Cough, trouble breathing, or fast breathing.
- Superior vena cava syndrome. This can cause coughing, trouble breathing, and swelling of the face, neck, and upper arms. For more information, see Cardiopulmonary Syndromes.
Endocrine system
Signs or symptoms of LCH that affects the pituitary gland may include:
- Diabetes insipidus. This can cause a strong thirst and frequent urination.
- Slow growth.
- Early or late puberty.
- Being very overweight.
Signs or symptoms of LCH that affects the thyroid may include:
- Swollen thyroid gland.
- Hypothyroidism. This can cause tiredness, lack of energy, being sensitive to cold, constipation, dry skin, thinning hair, memory problems, trouble concentrating, and depression. In infants, this can also cause a loss of appetite and choking on food. In children and adolescents, this can cause behavior problems, weight gain, slow growth, and late puberty.
- Trouble breathing.
Eye
Signs or symptoms of LCH that affects the eye may include:
- Vision problems or blindness.
Central nervous system (CNS)
Signs or symptoms of LCH that affects the CNS (brain and spinal cord) may include:
- Loss of balance, uncoordinated body movements, and trouble walking.
- Trouble speaking.
- Trouble seeing.
- Headaches.
- Changes in behavior or personality.
- Memory problems.
These signs and symptoms may be caused by lesions in the CNS or by CNS neurodegenerative syndrome.
Liver and spleen
Signs or symptoms of LCH that affects the liver or spleen may include:
- Swelling in the abdomen caused by a buildup of extra fluid.
- Trouble breathing.
- Yellowing of the skin and whites of the eyes.
- Itching.
- Easy bruising or bleeding.
- Feeling very tired.
- Diarrhea.
- Bloody stools.
Lung
Signs or symptoms of LCH that affects the lung may include:
- Collapsed lung. This condition can cause chest pain or tightness, trouble breathing, feeling tired, and a bluish color to the skin.
- Trouble breathing, especially in adults who smoke.
- Dry cough.
- Chest pain.
Bone marrow
Signs or symptoms of LCH that affects the bone marrow may include:
- Easy bruising or bleeding.
- Fever.
- Frequent infections.
Tests that examine the organs and body systems where LCH may occur are used to diagnose LCH.
In addition to asking about your health history and doing a physical exam, your doctor may perform the following tests and procedures to diagnose LCH or conditions caused by LCH:
-
Complete blood count (CBC) with differential: A procedure in which a sample of blood is drawn and checked for the following:
- The amount of hemoglobin (the protein that carries oxygen) in the red blood cells.
- The portion of the blood sample made up of red blood cells.
- The number and type of white blood cells.
- The number of red blood cells and platelets.
- Blood chemistry studies: A procedure in which a blood sample is checked to measure the amounts of certain substances released into the body by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Liver function test: A blood test to measure the blood levels of certain substances released by the liver. A high or low level of these substances can be a sign of disease in the liver.
- BRAFgene testing: A laboratory test in which a sample of blood or tissue is tested for certain mutations in the BRAF gene.
- Urinalysis: A test to check the color of urine and its contents, such as sugar, protein, red blood cells, and white blood cells.
- Water deprivation test: A test to check how much urine is made and whether it becomes concentrated when little or no water is given. This test is used to diagnose diabetes insipidus, which may be caused by LCH.
-
Bone marrow aspiration and biopsy: The removal of bone marrow and a small piece of bone by inserting a hollow needle into the hipbone. A pathologist views the bone marrow and bone under a microscope to look for signs of LCH.
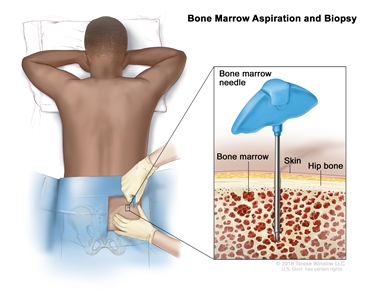
Bone marrow aspiration and biopsy. After a small area of skin is numbed, a long, hollow needle is inserted through the patient's skin and hip bone into the bone marrow. A sample of bone marrow and a small piece of bone are removed for examination under a microscope.The following test may be done on the tissue that was removed:
- Immunohistochemistry: A laboratory test that uses antibodies to check for certain antigens (markers) in a sample of a patient's tissue. The antibodies are usually linked to an enzyme or a fluorescent dye. After the antibodies bind to a specific antigen in the tissue sample, the enzyme or dye is activated, and the antigen can then be seen under a microscope. This type of test is used to help diagnose cancer and to help tell one type of cancer from another type of cancer.
-
Bone scan: A procedure to check if there are rapidly dividing cells in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in the bones with LCH and is detected by a scanner.
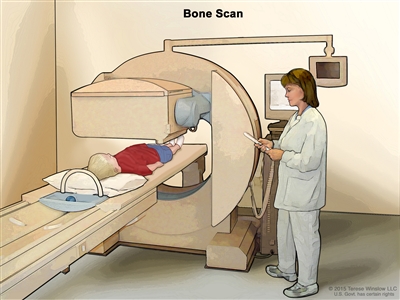
Bone scan. A small amount of radioactive material is injected into the child's vein and travels through the blood. The radioactive material collects in the bones. As the child lies on a table that slides under the scanner, the radioactive material is detected and images are made on a computer screen. - X-ray: An x-ray of the organs and bones inside the body. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body. Sometimes a skeletal survey is done. This is a procedure to x-ray all the bones in the body.
-
CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
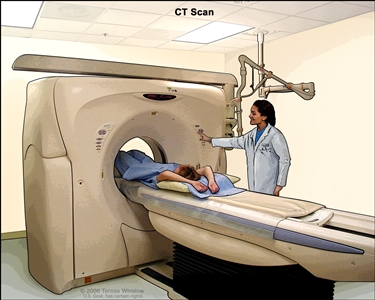
Computed tomography (CT) scan of the abdomen. The patient lies on a table that slides through the CT machine, which takes x-ray pictures of the inside of the body. -
MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. A substance called gadolinium may be injected into a vein. The gadolinium collects around the LCH cells so that they show up brighter in the picture. This procedure is also called nuclear magnetic resonance imaging (NMRI).
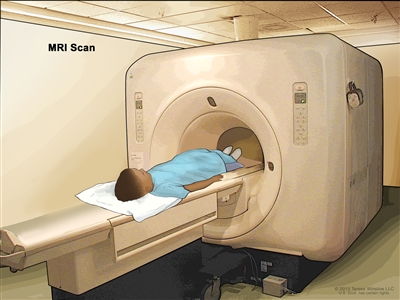
Magnetic resonance imaging (MRI) scan. The child lies on a table that slides into the MRI machine, which takes a series of detailed pictures of areas inside the body. The positioning of the child on the table depends on the part of the body being imaged. -
PET scan (positron emission tomography scan): A procedure to find tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do.
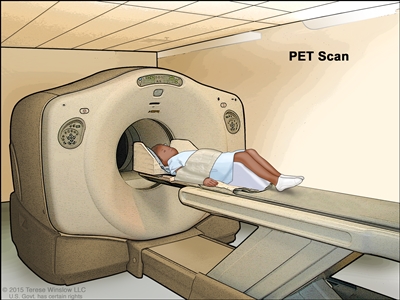
Positron emission tomography (PET) scan. The child lies on a table that slides through the PET scanner. The head rest and white strap help the child lie still. A small amount of radioactive glucose (sugar) is injected into the child's vein, and a scanner makes a picture of where the glucose is being used in the body. Cancer cells show up brighter in the picture because they take up more glucose than normal cells do. -
Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to be looked at later.
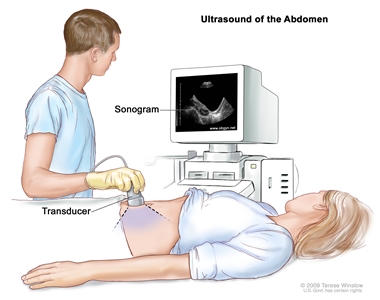
Abdominal ultrasound. An ultrasound transducer connected to a computer is passed over the surface of the abdomen. The ultrasound transducer bounces sound waves off internal organs and tissues to make echoes that form a sonogram (computer picture). - Pulmonary function test (PFT): A test to see how well the lungs are working. It measures how much air the lungs can hold and how quickly air moves into and out of the lungs. It also measures how much oxygen is used and how much carbon dioxide is given off during breathing. This is also called lung function test.
- Bronchoscopy: A procedure to look inside the trachea and large airways in the lung for abnormal areas. A bronchoscope is inserted through the nose or mouth into the trachea and lungs. A bronchoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of LCH.
- Endoscopy: A procedure to look at organs and tissues inside the body to check for abnormal areas in the gastrointestinal tract or lungs. An endoscope is inserted through an incision (cut) in the skin or opening in the body, such as the mouth. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of disease.
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for LCH cells. To diagnose LCH, a biopsy of bone, skin, lymph nodes, liver, or other sites of disease may be done.
Certain factors affect prognosis (chance of recovery) and treatment options.
LCH in organs such as the skin, bones, lymph nodes, or pituitary gland usually gets better with treatment and is called "low-risk." LCH in the spleen, liver, or bone marrow is harder to treat and is called "high-risk." Children with LCH in high-risk organs and the gastrointestinal tract have a greater risk of not responding to treatment than patients with high-risk LCH and no disease in the gastrointestinal tract. High-risk LCH is usually seen in children younger than 2 years.
The prognosis and treatment options depend on the following:
- Which organs or body systems are affected by LCH.
- How many organs or body systems the LCH affects.
- Whether LCH is found in the liver, spleen, bone marrow, or certain bones in the skull.
- How quickly LCH responds to initial treatment.
- Whether there are certain mutations in the BRAF gene.
- Whether LCH has just been diagnosed or has come back (recurred).
In infants up to 1 year of age, LCH may go away without treatment.
Stages of LCH
There is no standard staging system for Langerhans cell histiocytosis (LCH).
The process used to find out if cancer has spread to other parts of the body is called staging. There is no standard staging system for LCH.
Treatment of LCH is based on where LCH cells are found in the body and whether the LCH is low risk or high risk.
LCH is described as single-system disease or multisystem disease, depending on how many body systems are affected:
- Single-system LCH: LCH is found in one part of an organ or body system or in more than one part of that organ or body system. Bone is the most common single place for LCH to be found.
- Multisystem LCH: LCH is found in two or more organs or body systems or may be found throughout the body. Multisystem LCH is less common than single-system LCH.
LCH may affect low-risk organs or high-risk organs:
- Low-risk organs include the skin, bone, lungs, lymph nodes, gastrointestinal tract, pituitary gland, thyroid gland, thymus, and central nervous system (CNS).
- High-risk organs include the liver, spleen, and bone marrow.
Sometimes LCH continues to grow or comes back after treatment.
Progressive LCH describes LCH that continues to grow, spread, or get worse. Progressive disease may be a sign that the LCH has become refractory to treatment.
Refractory LCH describes LCH that does not respond to initial treatment.
Recurrent or reactivated LCH describes LCH that has come back after it has been treated.
Many patients with LCH get better with treatment. However, when treatment stops, new lesions may appear or old lesions may come back. This is called reactivation (recurrence) and may occur within 1 year after stopping treatment. Patients with multisystem disease are more likely to have a reactivation. Common sites of reactivation are bone, ears, or skin. Diabetes insipidus also may develop. Less common sites of reactivation include lymph nodes, bone marrow, spleen, liver, or lung. Some patients may have more than one reactivation.
Treatment Option Overview for LCH
There are different types of treatment for patients with Langerhans cell histiocytosis (LCH).
Different types of treatments are available for patients with LCH. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Whenever possible, patients should take part in a clinical trial in order to receive new types of treatment for LCH. Some clinical trials are open only to patients who have not started treatment.
Clinical trials are taking place in many parts of the country. Information about ongoing clinical trials is available from the NCI website. Choosing the most appropriate treatment is a decision that ideally involves the patient, family, and health care team.
Children with LCH should have their treatment planned by a team of health care providers who are experts in treating childhood cancer or LCH.
Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other pediatric health care providers who are experts in treating children with LCH and who specialize in certain areas of medicine. These may include the following specialists:
- Pediatrician.
- Pediatric surgeon.
- Pediatric hematologist.
- Radiation oncologist.
- Neurologist.
- Endocrinologist.
- Pediatric nurse specialist.
- Rehabilitation specialist.
- Psychologist.
- Social worker.
Nine types of standard treatment are used to treat LCH.
Although it is unknown whether LCH is a type of cancer, some of the treatments used for cancer are effective at treating LCH.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. Chemotherapy that is taken by mouth or injected into a vein or muscle enters the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). Chemotherapy may also be applied to the skin in a cream or lotion (topical chemotherapy).
Chemotherapy may be given by injection, by mouth, or applied to the skin to treat LCH.
Surgery
Surgery may be used to remove LCH lesions and a small amount of nearby healthy tissue. Curettage is a type of surgery that uses a curette (a sharp, spoon-shaped tool) to scrape LCH cells from bone.
When there is severe liver or lung damage, the entire organ may be removed and replaced with a healthy liver or lung from a donor.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. Ultraviolet B (UVB) radiation therapy may be given using a special lamp that directs radiation toward LCH skin lesions.
Photodynamic therapy
Photodynamic therapy is a cancer treatment that uses a drug and a certain type of laser light to kill cancer cells. A drug that is not active until it is exposed to light is injected into a vein. The drug collects more in cancer cells than in normal cells. For LCH, laser light is aimed at the skin and the drug becomes active and kills the cancer cells. Photodynamic therapy causes little damage to healthy tissue. Patients who have photodynamic therapy should not spend too much time in the sun.
In one type of photodynamic therapy, called psoralen and ultraviolet A (PUVA) therapy, the patient receives a drug called psoralen and then ultraviolet A radiation is directed to the skin.
Immunotherapy
Immunotherapy is a treatment that uses the patient's immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body's natural defenses against cancer. Thalidomide is a type of immunotherapy used to treat LCH.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. There are different types of targeted therapy:
- BRAF inhibitors block proteins needed for cell growth and may kill cancer cells. The BRAFgene is found in a mutated (changed) form in some LCH and blocking it may help keep LCH cells from growing.
- Vemurafenib and dabrafenib are BRAF inhibitors used to treat LCH.
- MEK inhibitors block proteins called MEK1 and MEK2 that affect the growth and survival of cancer cells.
- Trametinib is a MEK inhibitor that is being studied in the treatment of certain childhood tumors for use alone or combined with dabrafenib.
- Monoclonal antibodies are immune system proteins made in the laboratory to treat many diseases, including cancer. As a cancer treatment, these antibodies can attach to a specific target on cancer cells or other cells that may help cancer cells grow. The antibodies are able to then kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells.
- Rituximab is a monoclonal antibody used to treat LCH.
Other drug therapy
Other drugs used to treat LCH include the following:
- Steroid therapy, such as prednisone, is used to treat LCH lesions.
- Bisphosphonate therapy (such as pamidronate, zoledronate, or alendronate) is used to treat LCH lesions of the bone and to lessen bone pain.
- Anti-inflammatory drugs are drugs (such as pioglitazone and rofecoxib) that are commonly used to decrease fever, swelling, pain, and redness. Anti-inflammatory drugs and chemotherapy may be given together to treat adults with bone LCH.
Stem cell transplant
Chemotherapy is given to kill cancer cells. Healthy cells, including blood-forming cells, are destroyed by the LCH treatment. Stem cell transplant is a treatment to replace the blood-forming cells. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient or a donor and are frozen and stored. After the patient completes chemotherapy, the stored stem cells are thawed and given back to the patient through an infusion. These stem cells grow into (and restore) the body's blood cells.
Observation
Observation is closely monitoring a patient's condition without giving any treatment until signs or symptoms appear or change.
New types of treatment are being tested in clinical trials.
Information about clinical trials is available from the NCI website.
Treatment for Langerhans cell histiocytosis may cause side effects.
To learn more about side effects that begin during treatment for cancer, visit Side Effects.
Side effects from cancer treatment that begin after treatment and continue for months or years are called late effects. Late effects of cancer treatment may include the following:
- Slow growth and development.
- Hormone imbalance.
- Hearing loss.
- Bone, tooth, liver, and lung problems.
- Changes in mood, feeling, behavior, learning, thinking, or memory.
- Second cancers, such as leukemia, lymphoma, retinoblastoma, Ewing sarcoma, brain or liver cancer.
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the effects cancer treatment can have on your child. For more information, see Late Effects of Treatment for Childhood Cancer.
Many patients with multisystem LCH have late effects caused by treatment or by the disease itself. These patients often have long-term health problems that affect their quality of life.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI's clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
LCH patients should be monitored for many years because of the risk of reactivation (recurrence). Some of the tests that were done to diagnose LCH may be repeated. This is to see how well the treatment is working and if there are any new lesions. These tests may include:
- Physical exam.
- Neurological exam.
- Ultrasound exam.
- MRI.
- CT scan.
- PET scan.
Other tests that may be needed include:
- Brain stem auditory evoked response (BAER) test: A test that measures the brain's response to clicking sounds or certain tones to detect some types of hearing loss.
- Pulmonary function test (PFT): A test to see how well the lungs are working. It measures how much air the lungs can hold and how quickly air moves into and out of the lungs. It also measures how much oxygen is used and how much carbon dioxide is given off during breathing. This is also called a lung function test.
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Treatment of Low-Risk LCH in Children
For information about the treatments listed below, see the Treatment Option Overview section.
Skin Lesions
Treatment of newly diagnosed childhood Langerhans cell histiocytosis (LCH) skin lesions may include:
- Observation. Young children with skin-only LCH lesions should be followed over a period of many years due to a risk of diabetes insipidus.
When severe rashes, pain, ulceration, or bleeding occur, treatment may include the following:
- Steroid therapy.
- Chemotherapy given by mouth or vein.
- Chemotherapy applied to the skin.
- Photodynamic therapy with psoralen and ultraviolet A (PUVA) therapy.
- UVB radiation therapy.
Lesions in Bones or Other Low-Risk Organs
Treatment of newly diagnosed childhood LCH bone lesions in the front, sides, or back of the skull, or in any other single bone may include:
- Surgery (curettage) with or without steroid therapy.
- Low-dose radiation therapy for lesions that affect nearby organs, or are painful and cannot be treated with other therapy.
Treatment of newly diagnosed childhood LCH lesions in bones around the ears or eyes is done to lower the risk of diabetes insipidus and other long-term problems. Treatment may include:
- Chemotherapy and steroid therapy.
- Surgery (curettage).
Treatment of newly diagnosed childhood LCH lesions of the spine or thigh bone may include:
- Observation.
- Low-dose radiation therapy.
- Chemotherapy, for lesions that spread from the spine into nearby tissue.
- Surgery to strengthen the weakened bone by bracing or fusing the bones together.
Treatment of two or more bone lesions may include:
- Chemotherapy and steroid therapy.
Treatment of two or more bone lesions combined with skin lesions, lymph node lesions, or diabetes insipidus may include:
- Chemotherapy with or without steroid therapy.
- Bisphosphonate therapy.
CNS Lesions
Treatment of newly diagnosed childhood LCH central nervous system (CNS) lesions may include:
- Chemotherapy with or without steroid therapy.
Treatment of newly diagnosed LCH CNS neurodegenerative syndrome may include:
- Targeted therapy with BRAF inhibitors (vemurafenib or dabrafenib).
- Chemotherapy.
- Targeted therapy with a monoclonal antibody (rituximab).
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of High-Risk LCH in Children
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of newly diagnosed childhood LCH multisystem disease lesions in the spleen, liver, or bone marrow and another organ or site may include:
- Chemotherapy and steroid therapy. Higher doses of more than one chemotherapy drug and steroid therapy may be given to patients whose tumors do not respond to initial chemotherapy.
- Targeted therapy (vemurafenib).
- A liver transplant for patients with severe liver damage.
- A clinical trial that tailors the patient's treatment based on features of the LCH at diagnosis and how it responds to treatment.
- A clinical trial of chemotherapy and steroid therapy.
Treatment of Progressive, Refractory, or Recurrent Childhood LCH in Children
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of progressive, refractory, or recurrent low-risk LCH may include:
- Chemotherapy with or without steroid therapy.
- Bisphosphonate therapy.
Treatment of progressive, refractory, or recurrent high-risk multisystem LCH may include:
- Chemotherapy.
- Targeted therapy (vemurafenib).
- Stem cell transplant.
Treatments being studied for progressive, refractory, or recurrent childhood LCH include the following:
- A clinical trial that tailors the patient's treatment based on features of the LCH at diagnosis and how it responds to treatment.
- A clinical trial of targeted therapy (trametinib and dabrafenib).
Treatment of LCH in Adults
Langerhans cell histiocytosis (LCH) in adults is a lot like LCH in children and can form in the same organs and systems as it does in children. These include the endocrine and central nervous systems, liver, spleen, bone marrow, and gastrointestinal tract. In adults, LCH is most commonly found in the lung as a single-system disease. In some patients, other organs may be involved, including bone, skin, hypothalamus, or pituitary gland. LCH in the lung occurs more often in young adults who smoke.
As in children, the signs and symptoms of LCH depend on where it is found in the body. See the General Information section for the signs and symptoms of LCH.
Tests that examine the organs and body systems where LCH may occur are used to detect (find) and diagnose LCH. See the General Information section for tests and procedures used to diagnose LCH.
In adults, there is not a lot of information about what treatment works best. Sometimes, information comes only from reports of the diagnosis, treatment, and follow-up of one adult or a small group of adults who were given the same type of treatment.
Adult patients with LCH have higher rates of other cancers than do adults of the same age without LCH. These cancers may be found before, at the same time, or after an LCH diagnosis, and occur more in patients who smoke.
For information about the treatments listed below, see the Treatment Option Overview section.
Lung Lesions
Treatment for LCH of the lung in adults may include:
- Quitting smoking. Lung damage will get worse over time in patients who do not quit smoking. In patients who quit smoking, lung damage may get better or it may get worse over time.
- Chemotherapy.
- Lung transplant for patients with severe lung damage.
- Steroid therapy.
Sometimes LCH of the lung will go away or not get worse even if it's not treated.
Bone Lesions
Treatment for LCH that affects only the bone in adults may include:
- Surgery with or without steroid therapy.
- Chemotherapy.
- Radiation therapy.
- Bisphosphonate therapy, for severe bone pain.
- Anti-inflammatory drugs (pioglitazone or rofecoxib) with chemotherapy.
Skin Lesions
Treatment for LCH that affects only the skin in adults may include:
- Surgery.
- Steroid or other drug therapy (tacrolimus or imiquimod) applied or injected into the skin.
- Photodynamic therapy with psoralen and ultraviolet A (PUVA) radiation.
- UVB radiation therapy.
- Chemotherapy or immunotherapy given by mouth, such as methotrexate, thalidomide, or hydroxyurea.
Treatment for LCH that affects the skin and other body systems in adults may include:
- Chemotherapy.
Single-System and Multisystem Disease
Treatment of single-system and multisystem disease in adults that does not affect the lung, bone, or skin may include:
- Chemotherapy.
- Radiation therapy.
- Targeted therapy (vemurafenib).
For more about LCH trials for adults, see the Histiocyte Society website.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Langerhans Cell Histiocytosis
For more from the National Cancer Institute about Langerhans cell histiocytosis treatment, see the following:
- Computed Tomography (CT) Scans and Cancer
- Photodynamic Therapy for Cancer
- Immunotherapy to Treat Cancer
- Targeted Therapy to Treat Cancer
- Stem Cell Transplants in Cancer Treatment
For more childhood cancer information and other general cancer resources, visit:
- About Cancer
- Childhood Cancers
- CureSearch for Children's Cancer
- Late Effects of Treatment for Childhood Cancer
- Adolescents and Young Adults with Cancer
- Children with Cancer: A Guide for Parents
- Cancer in Children and Adolescents
- Cancer Staging
- Coping with Cancer
- Questions to Ask Your Doctor about Cancer
- For Survivors, Caregivers, and Advocates
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of childhood and adult Langerhans cell histiocytosis. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Langerhans Cell Histiocytosis Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/langerhans/patient/langerhans-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389196]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2024-06-06
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.


